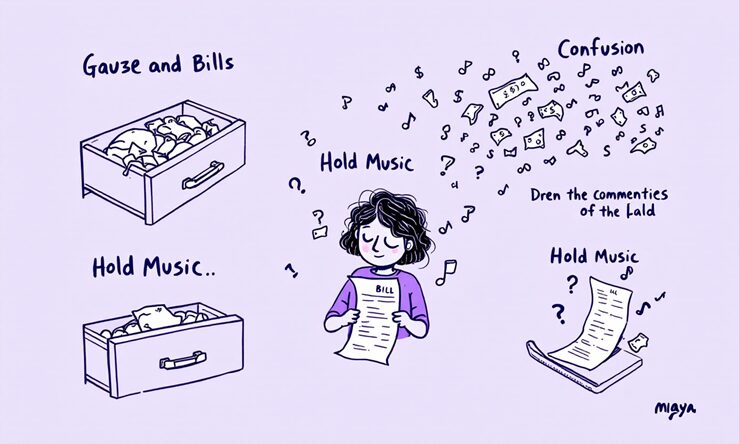
It starts quietly, almost unnoticeable at first—a federal policy tweak somewhere distant, maybe debated in a windowless room, and then months later, Maya is still waiting for anything to shift in her small rural town. There’s this odd gap, something that feels like time stretching out thin; someone hears about the change on the news or from a friend who heard it from their cousin who works at a clinic. Vero follows along, tracking how these adjustments wander down through layers of state paperwork and local offices before they ever brush up against caregivers’ reality. By the time Maya actually feels it—sometimes half a year on—the details have blurred and nobody’s quite sure what was supposed to happen versus what did. People guess, double-check old emails, wonder if they missed something important. Meanwhile, she keeps doing what she’s always done: showing up before sunrise because her clients can’t wait for bureaucracy to catch up. Out here it’s not just about rules changing overnight; it’s more like watching dominoes fall in slow motion, with some never tipping over at all. The confusion settles in quietly too, mixing with daily routines until everyone forgets there was ever another way things worked—or could wor
“Hold on, that changed everything?” Maya almost laughs, but not really. One day things are fine—her client’s prescriptions go through without a hitch—and then out of nowhere, the pharmacy says no, coverage’s shifted. Maybe it was an email she missed? Or some vague memo from the state that got buried under other messages? She tries to piece together what happened, scrolling old notifications and half-remembered news about policy tweaks. In rural clinics, they say these delays can drag on for months before anyone even notices something’s different. Confusion creeps in; clients call her up wondering if she knows more than they do. Most times, she doesn’t—nobody does until suddenly everyone does, all at once or not at all.
It’s strange how policies on paper always seem so far removed from the morning scramble—until suddenly, they aren’t. Maya remembers one day when her phone wouldn’t stop buzzing with questions about a medication that had always been routine, now tangled up because of some new rule she hadn’t even heard about until that week. The abrupt shift felt like someone rearranged the furniture overnight and forgot to mention it. Maybe this happens every year, maybe just every few; nobody seems sure. Friends in other counties say these surprises can take over seventy days to really take effect, sometimes even longer if you’re out where mail comes late and rumors move faster than official notices. One minute she’s sorting pillboxes, next she’s stuck piecing together what changed and why it matters.
It’s almost as if a single pebble tossed in a pond sends out ripples that won’t quit, only these ripples take their time—sometimes meandering for weeks, maybe longer. Imagine Maya watching the first policy notice drop; she can practically hear invisible dominoes toppling somewhere out of sight, slow-motion style. The rule changes don’t arrive all at once—they trickle down oddly, like rainclouds that promise relief but end up missing half the fields. By the time any difference actually reaches her town or her client’s doorstep, it’s hard to remember what triggered the whole thing. Folks swap stories about delays over grocery lines, unsure if next week will finally bring what everyone expected months ago—or just more waiting layered on top.
Somewhere between sunrise and the first coffee, numbers start to blur for people like Maya. It’s not just one report or a single year—over several cycles, data from Vero and other organizations have circled around the same uneasy truth: most caregivers find themselves stretched thin, with maybe 70% saying they’ve had to choose between buying medication and buying groceries at some point. The lines aren’t clear-cut. Some surveys hint that nearly half of respondents admit to skipping meals now and then just to keep up with supply costs, but others recall only “a lot” or “almost always” when pressed for details. The actual prevalence probably falls somewhere in-between, depending on how you define things like ‘sacrifice’ or ‘need.’ There are also studies floating around suggesting caregivers in more remote areas get hit hardest—possibly facing delays dozens of times longer than those in urban regions before they feel the effects of new policies. Financial strain is mentioned a lot, but it mixes together with uncertainty over what benefits will actually arrive this month or next. And while official reports try to pin down exact percentages for burnout or turnover, stories from folks like Maya tend to fill in the gaps—sometimes making it seem even more widespread than the charts suggest.
Sometimes, it’s the little shifts—like swapping a notebook for a whiteboard on the fridge—that make Maya’s mornings run smoother. Vero tossed out this idea after hearing how post-policy changes left caregivers scrambling for updates. There are these state health alerts, sure, but figuring out what matters isn’t always obvious; one email might be urgent, another just background noise. Maya started using color-coded sticky notes—maybe not everyone’s thing, but it helps her spot medication denials before they snowball. A friend swears by group texts with coworkers to share insurer news fast, though that can get messy if someone forgets to mute their phone at night. No perfect system exists, but piecing together these workarounds means folks like Maya aren’t flying completely blind while the official channels catch up—or don’t. (If you’d like to dive deeper, click here.)
So, maybe the real question isn’t just about rules coming down from some office miles away, but something else nobody can quite pin down—who actually catches Maya and people like her when things get rough? There’s this odd fog around where help is supposed to come from; sometimes it looks like community health offices, sometimes it’s a neighbor with leftover supplies, or just the hope that someone reads those policy updates before things break. You hear stories—someone tried calling an official helpline and got bounced between three different numbers, or there’s a grant you sort of hear about after it closed. It doesn’t add up easily. The support network for caregivers looks stitched together out of luck and habit more than anything designed. One week folks feel seen, next week everyone’s invisible again. How is anyone supposed to plan for tomorrow if today keeps changing shape? In all this shuffle—agencies shifting responsibility like they’re passing a hot potato—the ground under Maya never feels steady. What does “support” even mean here? Maybe no one ever figured that out in the first place, or maybe they did and forgot to tell the people who need it most.