Roja Rani Perumandla introduces a visionary model to embed social determinants into everyday clinical care
In today’s digital transformation era, healthcare is evolving to prioritize Social Determinants of Health (SDOH) as central elements in care delivery. Roja Rani Perumandla, an expert in healthcare systems, presents a groundbreaking framework that transforms social risk data into structured, actionable interventions. Her work offers a comprehensive roadmap that integrates community needs, advanced technology, and operational protocols to improve patient outcomes and support long-term health equity across diverse populations.
Historically, medical care has often overlooked the critical influence of social determinants of health (SDOH)—such as food insecurity, housing instability, transportation barriers, and unsafe living conditions. These non-clinical factors have a profound impact on health outcomes, particularly in underserved communities. Drawing on insights from Eastern Illinois University, there is a growing emphasis on integrating these social variables into clinical systems. This approach leverages technology, fosters collaboration, and deepens the understanding of patients’ social environments to drive transformative change in healthcare delivery.
A Unified Snapshot of Impact: The Power of Numbers
86% of patients completed the Core 5 screening when workflows were standardized.
92% completion was achieved when integrated into vital sign collection.
76% was the rate when screening was limited to waiting room assessments.
40% higher screening was seen in teams with dedicated SDOH champions.
30% more actionable needs were identified with standardized documentation.
50% improvement in referral follow-through came from CHW involvement.
63% better financial performance was reported under value-based care platforms.
These figures reflect the powerful synergy between structured workflows, community collaboration, and data-driven systems in advancing social care delivery within modern healthcare.
Precision Meets People: Screening and Operational Integration
The Core 5 screening methodology targets five crucial social risk domains: food insecurity, housing instability, transportation barriers, utility needs, and interpersonal safety. Designed for speed and efficiency, it allows seamless data collection during clinical encounters. Its effectiveness lies in a human-centered approach that blends automation with compassionate care. The model thrives on clearly defined team roles, structured workflows, and ongoing staff training, creating a system where social determinants of health are addressed with the same urgency as medical issues. This fosters a responsive care environment where patients’ social needs are not overlooked but prioritized, ensuring comprehensive support. By integrating these practices, the Core 5 methodology builds a healthcare framework that identifies, responds to, and resolves social risks, enhancing overall patient well-being and improving health outcomes through coordinated and empathetic care delivery.
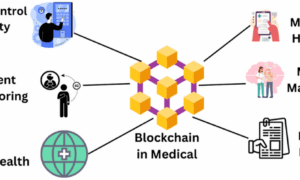
Tech-Driven Teams: Data, AI, and Care Management
The fusion of data systems with care coordination platforms has brought a new level of precision to social care. Electronic Health Records (EHRs) have been enhanced with person-centered models that link medical data with social insights. Predictive analytics, machine learning, and natural language processing allow care teams to move from reactive interventions to proactive support. These technologies empower care managers with real-time intelligence, enabling them to prioritize resources, track outcomes, and reduce redundancy. The result is a faster, smarter, and more scalable approach to delivering care.
Partnerships and Sustainability: Community at the Core
A defining strength of the framework lies in its deep commitment to community collaboration, enabling healthcare systems to engage directly with trusted local partners. Through these alliances, providers access updated resource directories, culturally tailored services, and strong trust networks, significantly enhancing care delivery. This collaborative approach expands the reach of medical services while promoting shared accountability. Moreover, by aligning with value-based reimbursement models, the framework ensures that social interventions are not only impactful but also measurable and financially sustainable. Ultimately, it repositions social care from an act of charity to a strategic investment in long-term health outcomes.
Conclusion: A Vision for Socially Integrated Care
Roja Rani Perumandla has developed a transformative framework that redefines how healthcare addresses the social determinants of health. Her model seamlessly blends technological precision, strong operational design, and deep community insight to create a system where social care is integral, not optional. By embedding these principles into everyday clinical practice, she champions a more equitable and responsive approach—ensuring that every patient’s social context is acknowledged and addressed as a vital part of their health journey.