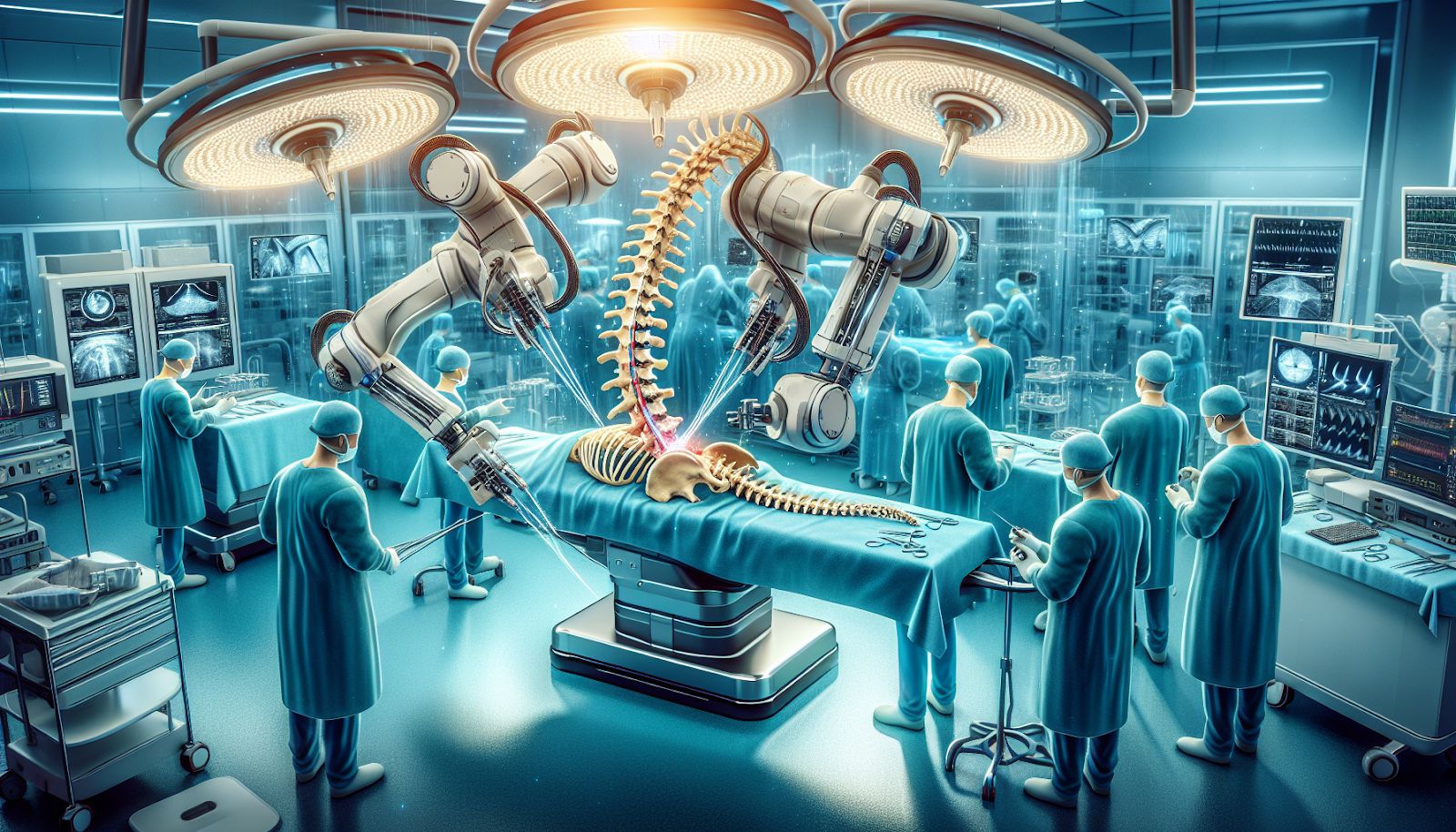
 Robotic Scoliosis Surgery represents a groundbreaking advance in the field of spine surgery, offering unprecedented precision in treating scoliosis, a condition characterized by an abnormal lateral curvature of the spine. This innovative approach leverages robotic systems, achieving accuracy in screw placement that rivals traditional methods. Such advancements are not only enhancing surgical outcomes but also promise a new era in spinal health care.
Robotic Scoliosis Surgery represents a groundbreaking advance in the field of spine surgery, offering unprecedented precision in treating scoliosis, a condition characterized by an abnormal lateral curvature of the spine. This innovative approach leverages robotic systems, achieving accuracy in screw placement that rivals traditional methods. Such advancements are not only enhancing surgical outcomes but also promise a new era in spinal health care.
This article delves into the evolution of Robotic Scoliosis Surgery, comparing it to traditional surgical techniques such as Spinal Fusion, and examining its economic viability. Through understanding these facets, readers will gain insight into what to expect from the future of robotic interventions in spine surgery and their potential benefits.
Understanding Scoliosis and Traditional Surgery Techniques
Scoliosis, a medical condition marked by an abnormal sideways curvature of the spine, primarily affects children and adolescents, especially just before puberty. The curvature, diagnosed when it exceeds 10 degrees, can occur in any of the spine’s three major sections: cervical (neck), thoracic (chest and upper back region), and lumbar (lower back). The treatment strategy for adolescent idiopathic scoliosis hinges on the curvature’s degree at diagnosis and its anticipated progression, with options ranging from observation in mild cases to nonsurgical methods like bracing or surgical interventions such as spinal fusion surgery.
Traditional Surgery Techniques:
- Spinal Fusion Surgery: The most common surgical intervention for more significant cases of scoliosis, spinal fusion, involves the welding of vertebrae together using bone chips. The alignment is maintained using hooks or screws and rods, allowing the spine to heal in the correct position. Typically, patients may need to stay in the hospital for three to five days and can usually return to school in four to six weeks. However, rare complications can include infection and spinal cord abnormalities or injury.
- Instrumentation Systems: Modern surgical treatments for scoliosis have evolved to use more anchors to connect the rod and the spine, leading to better correction of the curvature and less frequent implant failures. Techniques include segmental pedicle screw constructs or hybrid constructs using pedicle screws, hooks, and wires.
- Anterior Instrumentation Surgery: Previously favored for thoracolumbar and lumbar scoliosis due to its better correction capabilities and shorter fusion levels, the popularity of anterior instrumentation has waned. This is due to the associated risks, such as the potential for thoracic aorta injury and adverse impacts on pulmonary function.
In the quest to improve outcomes for scoliosis patients, various attempts at developing fusionless surgery techniques are underway. These innovative approaches include epiphysiodesis on the deformity’s convex side, with or without instrumentation, vertebral wedge osteotomies, and dual rod instrumentation. These advancements reflect the ongoing effort to minimize risks and improve the quality of life for individuals undergoing scoliosis treatment, setting the stage for a comparison with the emerging field of robotic scoliosis surgery.
The Evolution of Robotic Surgery in Treating Scoliosis
Robotic spine surgery, particularly in the treatment of scoliosis, has marked a significant evolution in spinal health care, offering a slew of benefits over traditional surgery techniques. The journey from manual to robotic-assisted procedures underscores a leap towards precision, safety, and personalized care.
Robotic Systems in Spinal Surgery: An Overview
- Accuracy in Pedicle Screw Placement: Studies have shown that robotic spine surgery significantly increases the accuracy of pedicle screw placement compared to conventional methods. This precision is crucial in scoliosis surgery, where the correct alignment of screws can dramatically affect the outcome.
- Clinical Advantages: Robotic-assisted surgery has been associated with several clinical benefits, including:
- Reduced intraoperative blood loss
- Lower radiation dose to patients
- Shorter hospital stays
- Applications and Benefits:
- Minimally Invasive Techniques: Robotic systems have expanded their applications, including minimally invasive procedures that result in less trauma and quicker recovery for patients.
- Deformity Correction: The technology has been particularly impactful in correcting spinal deformities, offering customized surgical plans based on individual patient needs.
Cost-Effectiveness and Training
- Despite the high initial costs associated with robotic systems, they could prove to be economically viable in the long run. The potential for reducing complications and hospital stays contributes to this cost-effectiveness. However, the widespread adoption of robotic systems in scoliosis surgery hinges on comprehensive training programs for surgeons and the willingness of healthcare providers to invest in this technology.
Future Prospects and Continued Research
- The future of robotic scoliosis surgery looks promising, with ongoing research and development aimed at improving existing technologies and introducing new ones. Robotic systems like the ExcelsiusGPS and SpineAssist have already shown favorable outcomes in various spinal procedures. The focus on automation and the potential for reducing the learning curve for pedicle screw insertion promise to make robotic surgery a mainstay in spinal health care.
Robotic scoliosis surgery represents a paradigm shift in treating spinal deformities, emphasizing the importance of precision, safety, and patient-specific care. As the technology continues to evolve, it holds the promise of transforming the landscape of spinal surgery, making procedures safer, more accurate, and potentially more accessible to a broader range of patients.
Comparing Surgical Outcomes: Robotic vs. Traditional Surgery
When comparing the outcomes of robotic scoliosis surgery to traditional surgery methods, several key points emerge from recent studies:
Accuracy and Efficiency:
- Robotic-Assisted Surgery: Shows a significant improvement in screw placement accuracy, operative efficiency, and reliability. A multicenter study highlighted these advancements, noting a substantial enhancement in outcomes and complications over a five-year period.
- Traditional Surgery: While effective, lacks the precision in screw placement that robotic assistance offers, potentially leading to longer operation times and increased risk of complications.
Clinical Outcomes:
- Blood Loss and Hospital Stay:
- Robotic Surgery: Patients experience less intraoperative blood loss and shorter hospital stays, indicating a smoother post-operative recovery.
- Traditional Surgery: Comparatively, patients tend to have higher rates of blood loss and longer hospital stays, impacting the overall recovery process.
- Radiation Exposure:
- Robotic Surgery: Utilizes lower doses of radiation, benefiting both patients and surgical teams.
- Traditional Surgery: Typically involves higher levels of radiation exposure due to the need for more frequent imaging during the procedure.
Efficacy and Patient Experience:
- Pain and Disability Scores: Both robotic and traditional surgery methods show similar outcomes in terms of pain relief and improvements in disability indexes. This suggests that while robotic surgery offers technical advantages, patient-centric outcomes like pain reduction and functional improvements are comparable between the two approaches.
- Learning Curve and Economic Benefits: Robotic surgery’s learning curve is acknowledged, with potential for decreased radiation exposure and economic advantages over time as proficiency improves.
In summary, robotic scoliosis surgery demonstrates clear advantages in terms of surgical precision, reduced intraoperative risks, and shorter hospitalization periods. However, when it comes to the overall clinical efficacy and patient experience, such as pain reduction and functional improvement, both robotic and traditional surgeries show similar outcomes. Further research into complications and cost-effectiveness is necessary to fully understand the long-term benefits and potential limitations of robotic surgery in the treatment of scoliosis.
Cost Analysis: Is Robotic Surgery Economically Viable?
Evaluating the economic viability of robotic-assisted lumbar spine fusion (rLF) compared to the traditional fluoroscopic freehand lumbar spine fusion (fLF) reveals a nuanced financial landscape. A detailed cost analysis based on recent studies sheds light on the initial and long-term financial implications of adopting robotic technology in spinal surgeries.
- Initial Costs Comparison:
- Robotic-Assisted Lumbar Spine Fusion (rLF): A case-control study highlighted significantly higher total encounter costs and day-of-surgery costs for rLF compared to fLF. The increased expenses were primarily due to the higher supply cost and operating room time cost.
- Total Encounter Costs: Higher for rLF (P < 0.001)
- Day-of-Surgery Costs: Higher for rLF (P = 0.005)
- Supply Cost: Increased in rLF (P = 0.0183)
- Operating Room Time Cost: Increased in rLF (P < 0.001)
- Fluoroscopic Freehand Lumbar Spine Fusion (fLF): Demonstrates lower initial costs in comparison, making it a financially appealing option for institutions with limited budgets.
- Long-term Savings and Efficiency:
- A comprehensive study published in Neurospine on 557 cases of robotic-assisted spine surgery revealed a total savings of $608,546 in one year, attributing to the cost-effectiveness of robotic surgery over time.
- The cost-per-case of employing a spinal robot, considering amortization and disposable instrumentation, stands at approximately $2,000, with a less than 1% risk rate.
- Enhanced operational efficiency was evident as the use of robotic technology resulted in an average time savings of 3.4 minutes per one-level MIS procedure. Furthermore, the improved accuracy in pedicle screw placement with robotic technology potentially avoided 9.47 revisions, translating to a cost savings of around $314,661.
- Impact on Patient Outcomes and Hospital Stays:
- The shift from open to minimally invasive procedures (MIS) facilitated by robotic technology could convert 31 Medicare and 18 commercial patients, leading to 140 fewer total hospital admission days and avoiding approximately 2.3 infections. This not only underscores the health benefits but also highlights the substantial economic advantage by reducing hospital stays and associated costs.
In summary, while the initial costs of robotic-assisted lumbar spine fusion are higher primarily due to increased supply and operating room time costs, the long-term financial analysis reveals significant savings. These savings are attributed to reduced revision rates, shorter hospital stays, and the conversion of procedures from open to minimally invasive, emphasizing the economic viability of robotic surgery in the broader context of healthcare economics.
The Future of Robotic Scoliosis Surgery
As robotic scoliosis surgery continues to evolve, the future holds promising advancements that may significantly impact how scoliosis is treated. These advancements are not only expected to refine surgical techniques but also to broaden the accessibility of high-quality care for patients worldwide. Here are some anticipated developments in the realm of robotic scoliosis surgery:
- Integration of Advanced Imaging Techniques:
- Enhanced Preoperative Planning: Utilizing 3D imaging and AI algorithms to simulate surgical outcomes, allowing surgeons to plan the procedure with unprecedented precision.
- Intraoperative Navigation: Real-time imaging feedback during surgery to adjust techniques, ensuring optimal screw placement and spinal alignment.
- Automation and Machine Learning:
- Predictive Analytics: Machine learning models that predict the progression of scoliosis and recommend personalized surgical interventions.
- Automated Instrumentation: Development of semi-autonomous robotic arms capable of performing specific surgical tasks under the supervision of a surgeon, potentially reducing operation times and human error.
- Global Accessibility and Training:
- Virtual Reality (VR) Training Modules: Surgeons around the world can train on virtual simulations of complex scoliosis cases, reducing the learning curve associated with robotic surgery.
- Telemedicine and Remote Surgery: Expanding the reach of skilled surgeons to remote areas, ensuring patients everywhere have access to advanced scoliosis treatment options.
These advancements are poised to revolutionize the field of spinal surgery, making procedures safer, more efficient, and more accessible. As research continues and technology advances, robotic scoliosis surgery may become the standard of care, offering hope to those suffering from this complex condition.
Conclusion
The landscape of scoliosis treatment is undergoing a transformative evolution, with robotic scoliosis surgery emerging as a beacon of hope for individuals grappling with this complex spinal condition. Through a synthesis of advanced imaging, unparalleled precision in surgical intervention, and the minimization of post-operative recovery times, this innovative approach underscores a significant leap forward in spinal health care. The comparative analysis revealing the juxtaposition of robotic and traditional surgery methodologies, alongside a detailed economic viability assessment, highlights the multifaceted benefits of opting for robotic surgery—from enhanced surgical outcomes to long-term healthcare savings.
As we anticipate the future, the integration of automation, machine learning, and global training initiatives promises to not only refine these surgical techniques but also expand their accessibility, fundamentally altering the scoliosis treatment paradigm. For individuals exploring treatment options, the journey towards a groundbreaking solution in spinal health care leads to esteemed establishments like Turan&Turan which are at the forefront of harnessing robotic technology for scoliosis surgery. Amidst ongoing research and technological enhancements, the commitment to advancing robotic systems in spinal surgery remains unwavering, heralding a new era of precision, safety, and personalized patient care in the battle against scoliosis.
FAQs
What makes robotic spine surgery beneficial?Robotic spine surgery is advantageous because it is typically shorter and less invasive than conventional open surgery. Patients often experience reduced hospital stays and a decreased need for narcotic pain medication post-operation. Additionally, this type of surgery aims to preserve the patient’s natural anatomy, including muscles, tendons, and ligaments.
Can you list three advantages of undergoing robotic surgery?Certainly, the three key advantages of robotic surgery over traditional open surgery are:
- Reduced duration of hospital stay.
- Less pain and discomfort following the procedure.
- Quicker recovery time, allowing patients to return to their normal activities sooner.
How long does it take to recover from robotic back surgery?On average, patients can expect a recovery period of about 4 to 6 weeks after minimally invasive robotic back surgery. During this time frame, most individuals are able to return to their daily activities and work. This is significantly shorter than the recovery time for traditional back surgery, which can sometimes extend to a year or more.
What potential risks are associated with scoliosis surgery?Scoliosis surgery, like any spinal operation, carries certain risks. These may include complications such as infections, nerve damage, excessive blood loss, and issues with bowel and bladder function. It’s important for patients to discuss these potential risks with their healthcare provider to make an informed decision about their treatment options.




























