Leaving the hospital is meant to bring a sense of relief. In reality, it often feels like stepping off a cliff with paperwork in one hand and instructions in the other. Recovery does not end at discharge. It changes location. The quality of that transition shapes outcomes more than most people realize.
Healthcare is slowly acknowledging this shift. Research shows that roughly 30–40 percent of care delivered in the U.S. can safely move into the home.
At the same time, a widely shared “Chart of the Century” shows hospital service prices rose more than 220 percent between 2000 and 2022. According to the Baker Institute, that growth outpaced every other category, including overall medical services and inflation. Home care is not just compassionate. It is practical.
Here’s how to make that transition work.
Start Planning Before Discharge
The transition begins before anyone packs a bag. Hospitals often move fast at discharge, but patients and families should slow the process down. Ask clear questions. What care is still needed? Who will provide it? What signs mean something is wrong?
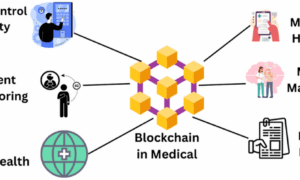
This is where skilled nursing services often enter the picture. Under physician guidance, skilled nurses can manage wound care, IV medications, injections, catheter care, and ongoing assessments at home.
They track vital signs, review medication responses, and document progress for physicians. As noted by Home Advantage Home Health Agency, they also educate patients and caregivers, turning complex medical instructions into manageable daily routines.
Before leaving, request a written care plan. It should list medications, dosages, therapy schedules, follow-up appointments, and emergency contacts. Do not rely on memory. Fatigue and stress distort details.
Understand the Medical Needs at Home
Home recovery is rarely straightforward, especially for older adults. According to the National Council on Aging, 79 percent of adults aged 65 live with two or more chronic conditions. Managing those conditions at home means coordinating medications, symptoms, mobility, and follow-up care at the same time.
That complexity makes realistic expectations essential. Some patients need daily monitoring, while others need structured check-ins and clear escalation plans. Home care can look very different depending on diagnoses, medications, and functional limits, so those details should be defined before discharge.
Medical needs often overlap and affect one another. Families should ask for hands-on demonstrations whenever possible. Seeing a nurse perform a task builds confidence that instructions cannot.
Prepare the Home Environment
Homes are not hospitals, and that difference matters during recovery. Most readmissions are triggered by small, preventable issues that start at home. Simple environmental changes can significantly reduce risk.
Clear walkways so mobility aids move easily. Remove loose rugs that catch feet or wheels. Improve lighting, especially along nighttime paths to the bathroom. Choose a recovery space close to essential rooms to limit unnecessary movement.
These adjustments are not cosmetic. They directly reduce fall risk, which remains one of the most common reasons patients return to the hospital. When setting up the home, think about access rather than aesthetics. Recovery favors simplicity. The priority is safety, stability, and ease of movement, not visual comfort or design preferences.
Manage Medications Carefully
Medication management becomes most fragile after discharge, when routines change, and oversight decreases. The risk is not minor.
Research cited by the National Library of Medicine indicates that medication-related errors account for approximately 5 to 40 percent of hospital admissions worldwide. They also account for about 22 percent of hospital readmissions after discharge. Those numbers reflect how easily small mistakes escalate.
This risk increases for older adults managing multiple prescriptions. Before leaving the hospital, request a complete medication reconciliation to confirm what has been stopped, continued, or newly prescribed.
At home, rely on pill organizers or digital reminders, not memory. Never adjust doses without guidance. If side effects, confusion, or unusual symptoms appear, report them immediately. Waiting often turns preventable issues into emergencies.
Watch for Warning Signs and Support Caregivers
Home recovery works best when problems are identified early, and support systems stay strong. Patients and caregivers should know which symptoms require attention. Warning signs vary by condition but often include fever, sudden pain changes, breathing difficulty, confusion, swelling, or unusual drainage.
Providers should clearly explain which symptoms need urgent care and which can be monitored. That clarity reduces anxiety and prevents unnecessary hospital visits while ensuring real issues are addressed quickly.
At the same time, home health care depends heavily on informal caregivers. Family members often manage complex tasks with little rest or training. Caregiver burnout directly affects recovery outcomes. Building in respite, accepting help, and rotating responsibilities matter. Professional home health services are not a failure. They strengthen the care team and support long-term recovery.
Balance Cost, Quality, and Ongoing Care
Recovery decisions are not only clinical. They are about finances. The widely shared “Chart of the Century” highlights how sharply hospital costs have risen, making extended inpatient care increasingly unsustainable.
When appropriate, home health care offers a different equation. It lowers costs without sacrificing quality, often leading to fewer readmissions, steadier recovery, and greater dignity for patients.
Insurance coverage varies, so financial questions should be addressed early. Understanding what services are covered, for how long, and under what conditions reduces stress during an already demanding period.
Recovery also changes over time. Needs shift. Progress stalls or accelerates. Schedule follow-up appointments before discharge whenever possible to reassess care plans and medications. If something is not working, speak up. Home care is designed to adapt, but only when adjustments are actively made.
FAQs
What do you mean by home health care?
Home health care refers to medical and supportive services provided in a patient’s home instead of a hospital or facility. It may involve nursing support, therapeutic services, medication oversight, and help with everyday tasks. The aim is to aid recovery, manage ongoing conditions, and allow patients to live safely and independently at home.
What do you call a nurse who visits your home?
A nurse who visits your home is typically called a home health nurse. Depending on the care needed, this may be a registered nurse or a licensed practical nurse. They provide medical care such as assessments, medication management, wound care, and coordination with physicians during home recovery.
How can you care for someone with dementia at home?
Supporting a person with dementia at home centers on creating routine, ensuring safety, and maintaining consistency in daily care. This includes maintaining predictable routines, simplifying the environment, managing medications, and ensuring supervision as cognitive abilities change. Professional home health support and caregiver respite also play an important role as needs progress.
Overall, the shift from hospital to home is not just about convenience. It reflects a bigger change in how care is delivered. As more care moves into homes, patients regain agency. Healing happens in familiar spaces. Risks are managed, not eliminated, but often reduced.
A successful transition requires planning, communication, and support. When those pieces align, home becomes more than a place to recover. It becomes part of the care itself. And for many patients, that makes all the difference.