The addiction treatment industry has traditionally relied on methods developed decades ago. Group therapy, 12-step programs, and residential stays formed the backbone of recovery for generations. But a quiet revolution is underway. Technology is transforming how treatment centers operate, how clinicians track progress, and how patients maintain sobriety long after leaving care. The results are promising enough that even the most traditional facilities are paying attention.
Treatment providers across the country are integrating digital tools into clinical workflows. Forward-thinking facilities now use electronic health records, telehealth platforms, and data analytics to personalize treatment in ways that weren’t possible ten years ago. This shift isn’t about replacing human connection with screens. It’s about giving clinicians better information and giving patients more support between sessions. The human element remains central, but technology amplifies its effectiveness.
Data-Driven Treatment Planning
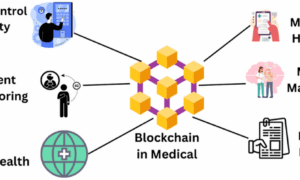
One of the most significant changes involves how treatment centers assess and monitor patients. Traditional intake processes relied heavily on self-reported information and clinical judgment. Both remain important, but they’re now supplemented by objective data that paints a fuller picture of each patient’s situation.
Wearable devices can track sleep patterns, heart rate variability, and physical activity levels. These metrics correlate with recovery outcomes in ways researchers are only beginning to understand. Poor sleep often precedes relapse. Elevated stress markers can signal vulnerability. Clinicians who have access to this data can intervene earlier, adjusting treatment plans before problems escalate rather than after.
The National Institute on Drug Abuse emphasizes that effective treatment must address multiple dimensions of a patient’s life. Technology makes this multidimensional approach more practical. When clinicians can see patterns across physical health, emotional state, and behavioral indicators, they can coordinate care more effectively. Treatment becomes less reactive and more predictive.
Telehealth Expands Access and Continuity
The pandemic accelerated telehealth adoption across all healthcare sectors, but the impact on addiction treatment has been particularly significant. Geographic barriers that once prevented people from accessing quality care have diminished. Someone living in a rural area with no nearby treatment facilities can now connect with specialists remotely. This matters enormously for a condition where timely intervention often determines outcomes.
Continuity of care has improved as well. The transition from residential treatment back to daily life has always been a vulnerable period. Patients leave structured environments and return to contexts filled with triggers and stressors. Telehealth bridges this gap by maintaining regular contact with treatment teams. Video sessions, check-in apps, and messaging platforms keep patients connected during the weeks and months when relapse risk peaks.
According to the Substance Abuse and Mental Health Services Administration, medication-assisted treatment combined with counseling produces the best outcomes for opioid use disorder. Telehealth makes this combination more accessible by allowing patients to receive counseling remotely while visiting local providers for medication management. The logistics that once made full-spectrum treatment difficult have become more manageable.
Digital Therapeutics Gain Clinical Validation
A newer category of technology, digital therapeutics, has started gaining FDA clearance for addiction treatment applications. These are software-based interventions designed to treat medical conditions, distinct from wellness apps that offer general support. The regulatory pathway signals that these tools meet clinical standards for safety and efficacy.
Prescription digital therapeutics for substance use disorders deliver cognitive behavioral therapy through smartphone apps. Patients complete modules, practice coping skills, and receive feedback between clinical appointments. Studies show these tools improve retention in treatment and reduce substance use days. They don’t replace traditional therapy but extend its reach into patients’ daily lives.
The business model for digital therapeutics is still evolving. Some products require prescriptions and work through insurance reimbursement. Others operate on subscription models or licensing agreements with treatment facilities. What’s clear is that the category is maturing beyond novelty status. Investors and healthcare systems are treating digital therapeutics as legitimate clinical tools rather than experimental add-ons.
Predictive Analytics and Early Warning Systems
Machine learning applications in addiction treatment remain in early stages but show considerable promise. Researchers are developing algorithms that analyze multiple data streams to predict relapse risk. These systems look at patterns in app usage, communication frequency, sleep data, and other indicators to flag patients who may need additional support.
The goal isn’t to automate clinical decisions but to help human clinicians prioritize their attention. A counselor managing dozens of patients can’t monitor everyone equally. Predictive tools can surface the cases that need immediate focus, allowing more efficient allocation of limited clinical resources. Early results suggest these systems catch warning signs that busy clinicians might otherwise miss.
Privacy considerations loom large in this space. Patients in recovery already face stigma and potential discrimination. Collecting detailed behavioral data raises legitimate questions about security, consent, and potential misuse. Treatment facilities implementing these technologies must balance clinical benefits against privacy risks, building systems that protect sensitive information while still enabling personalized care.
The Human Element Remains Essential
Technology enthusiasts sometimes oversell digital solutions as replacements for traditional care. In addiction treatment, this framing misses the point entirely. Recovery fundamentally involves human connection, accountability, and relationships. No app substitutes for a counselor who knows your history. No algorithm replaces the support of peers who understand your struggle firsthand.
What technology does well is remove friction from the treatment process. It makes scheduling easier, tracking more accurate, and communication more consistent. It extends the reach of skilled clinicians and fills gaps in the care continuum. Rehab staff from Arms Acres and similar facilities have found that the best implementations enhance human relationships rather than replacing them.
Treatment centers that thrive in the coming years will likely be those that integrate technology thoughtfully rather than adopting every new tool indiscriminately. They’ll use data to inform decisions without reducing patients to metrics. They’ll offer telehealth options while maintaining in-person connection for those who need it. The balance requires judgment that technology itself cannot provide.
Looking Ahead
Investment in addiction treatment technology continues to grow. Venture capital has flowed into digital health startups focused on behavioral health and substance use. Established healthcare systems are building or acquiring digital capabilities. The regulatory environment is adapting to accommodate new treatment modalities while maintaining safety standards.
For patients and families navigating addiction, these developments offer reason for cautious optimism. Access to quality care is expanding. Treatment approaches are becoming more personalized. The tools available to clinicians are improving. None of this makes recovery easy, but it does make effective treatment more attainable for more people.
The technology revolution in addiction treatment isn’t about flashy apps or futuristic promises. It’s about incremental improvements that compound over time. Better data leads to better decisions. Easier access leads to earlier intervention. More support between sessions leads to stronger recovery. These unglamorous gains add up to meaningful progress against a problem that has resisted simple solutions for far too long.