Technology is advancing rapidly, and with its advancement comes innovation into everyday life.
However, it’s not only work, home, or school that benefits from these technologies—various sectors have found ways to improve their operations through tech advancements like AI and machine learning.
One of those sectors is healthcare.
In 2021 alone, the global economy spent a staggering $9.8 trillion on healthcare, accounting for 10.3% of the global GDP.
Yet, despite this immense investment, critical inefficiencies persist—particularly in clinical trials and remote patient monitoring at an enterprise level. Clinical trials, essential for bringing new treatments to market, often suffer from slow patient recruitment, high dropout rates, and data silos that hinder real-time insights.
Meanwhile, enterprise-wide implementation of remote patient monitoring (RPM) faces challenges, such as integration with legacy systems, data security concerns, and inconsistent regulatory frameworks across regions.
However, digital health solutions reshape this landscape. Technologies like RPM kits address these inefficiencies by enabling continuous data collection, reducing the burden on in-person trials, and enhancing interoperability between healthcare systems. Patients benefit from more personalized, cost-effective treatments, while providers gain access to real-time health metrics that improve decision-making.
But the impact extends beyond patient care—these advancements also streamline research processes, enhance operational efficiency, and set the foundation for a more connected and effective healthcare ecosystem.
Traditionally, remote patient monitoring relied on intermittent data collection through manual check-ins or basic wearable devices—limiting real-time insights and delaying critical interventions. These fragmented approaches often left providers with incomplete patient health records, making proactive care difficult.
Today, in comparison, health solutions have redefined RPM by leveraging continuous tracking and real-time data integration. With technologies like the Internet of Things (IoT), healthcare providers can now monitor patients remotely with greater precision, detect anomalies earlier, and deliver more personalized treatments. This shift enhances patient outcomes and streamlines healthcare operations—making service delivery more proactive, efficient, and scalable.
As digital health solutions redefine remote patient monitoring, the focus shifts toward accessibility and scalability.
Patients need intuitive tools that provide real-time health insights without technical complexity, while healthcare institutions require solutions that integrate seamlessly with existing systems and scale efficiently.
Recognizing these needs, Mason developed RPM solutions that bridge the gap—offering user-friendly interfaces for patients while equipping providers with robust, configurable platforms that support rapid expansion. By addressing patient expectations and enterprise-level demands, we designed technology for researchers to incorporate RPM into decentralized clinical trials.
I’m Kaushlendra Tripathi, a Lead Android engineer. In this article, I’ll discuss how remote patient monitoring makes healthcare accessible, convenient, and beneficial to providers and patients and elaborate upon what we have built here at Mason that truly fulfills the need of the enterprise.
The Evolution of Digital Healthcare
Technology continues to reshape every aspect of our lives, including how we manage our health. The rise of digital health tools, such as Bluetooth-enabled Remote Patient Monitoring (RPM) devices, proves this transformation.
However, many early RPM solutions lacked seamless integration—making it difficult for healthcare providers to utilize patient data effectively.
Original Equipment Manufacturers (OEMs) have since recognized this gap—launching Bluetooth-enabled medical services to improve accessibility and accuracy. Despite these advancements, many of these products still struggle with inoperability.
We addressed this challenge by developing a fully integrated RPM solution that connects effortlessly with Bluetooth medical devices, ensuring real-time data transmission between patients and healthcare providers.
During the COVID-19 pandemic, consumers increasingly relied on in-home medical devices to monitor their health. With lockdowns and social distancing in place, they needed a way to share critical health data with doctors remotely.
However, many standalone devices lacked connectivity, making it difficult to transmit real-time patient data for timely medical decisions. Mason’s platform solved this issue by enabling seamless data sharing, allowing doctors to access patient vitals and provide informed care without in-person visits.
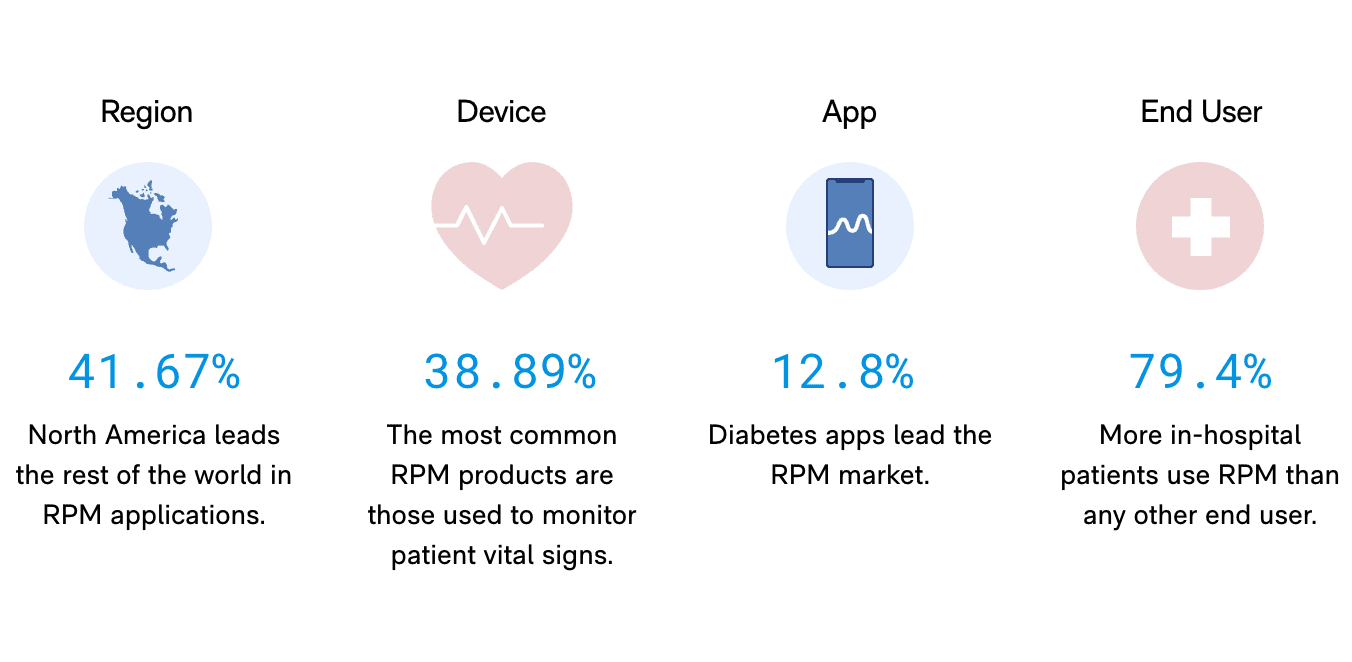
RPM by the Numbers – (Source: digitalscientists.com)
Beyond connectivity, artificial intelligence (AI) and machine learning (ML) have played a crucial role in enhancing digital healthcare. By integrating AI-driven analytics into its platform, Mason enables predictive health monitoring, helping providers detect early warning signs of potential health risks.
This proactive approach improves patient outcomes, reduces hospital readmissions, and optimizes healthcare resources.
As digital healthcare continues to evolve, the demand for seamless, integrated solutions will only grow. Mason remains at the forefront of this transformation, bridging the gap between patients, providers, and technology to create a more connected, efficient, and patient-centered healthcare system.
A Better Patient Experience with Remote Patient Monitoring
When I started my engineering career, I developed and improved services for various industries, such as travel, smartphones, and financial services.
Then, I discovered healthcare technology.
Seeing how technology improves delivery of healthcare services firsthand amazed me, and I realized I wanted to contribute to this cause.
With this objective in my mind, I focused on Remote Patient Monitoring (RPM). I saw how patients struggle with healthcare—from long wait times to expensive hospital stays and reactive care—and I knew RPM could change that.
With RPM, we can prevent patients from being readmitted to the hospital and their complications from worsening. An Agency for Healthcare Research and Quality (AHRQ) study pointed out that these systems promise improving outcomes for patients with chronic conditions, such as:
- Heart Disease
- Diabetes
- Chronic Obstructive Pulmonary Disease (COPD)
- Hypertension.
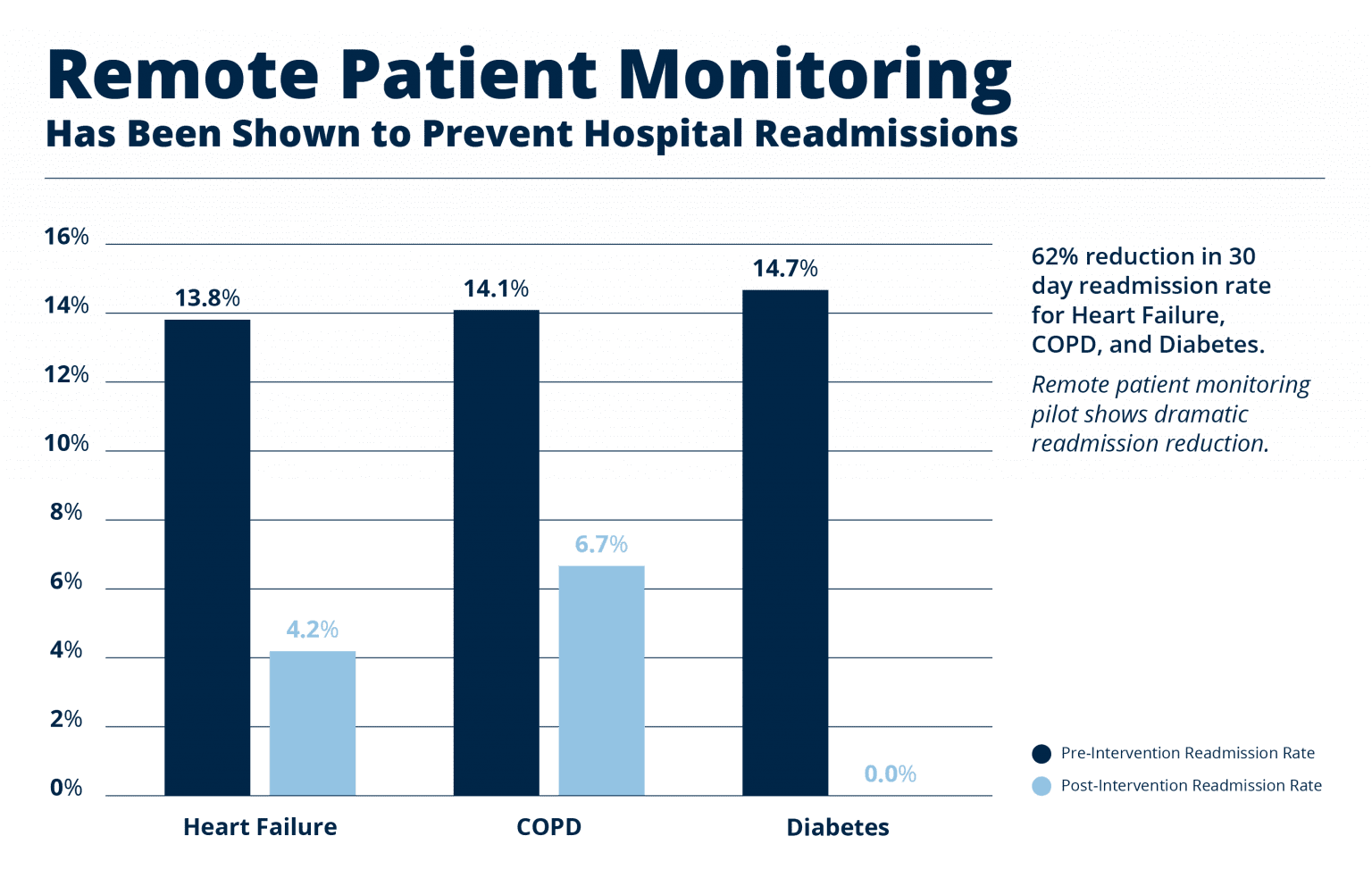
Readmission Percentage for People Using RPM – (Source: focusmd.net)
Take a hypertension patient, for example. They can continuously monitor their blood pressure using RPM and report any unusual spike triggers to their doctor. RPM enables the doctor to adjust the care plan immediately, which is impossible with traditional care models.
But what about patients and their families? What are they getting from using RPM?
In addition to the less frequent in-person visits, RPM allows patients to save time and reduce their financial burden. It takes healthcare into patients’ hands, transforming their approach to healthcare from reactive to proactive.
With this control and freedom, patients’ families become more at peace with their loved one’s condition. RPM has dashboards that update in real time, notifying family members of any changes, good or bad, anytime, adding an extra layer of security.
Moreover, healthcare providers can also benefit from RPM. Using RPM, we can prioritize patients who need immediate attention while automating routine tasks for stable cases so they can focus on where they’re needed most.
For example, AHRQ reports that Remote Patient Monitoring provides medical personnel with continuous data, making it easier to track trends, predict potential health issues, and improve chronic disease management.
However, the most impactful change that RPM brings lies in patient outcomes. These solutions catch issues early, preventing preventable hospitalization for people.
In short, RPM improves patients’ quality of life and reduces healthcare costs—making healthcare more personalized and patient-centric.
Dissecting RPM: Mason’s Modular RPM Kit
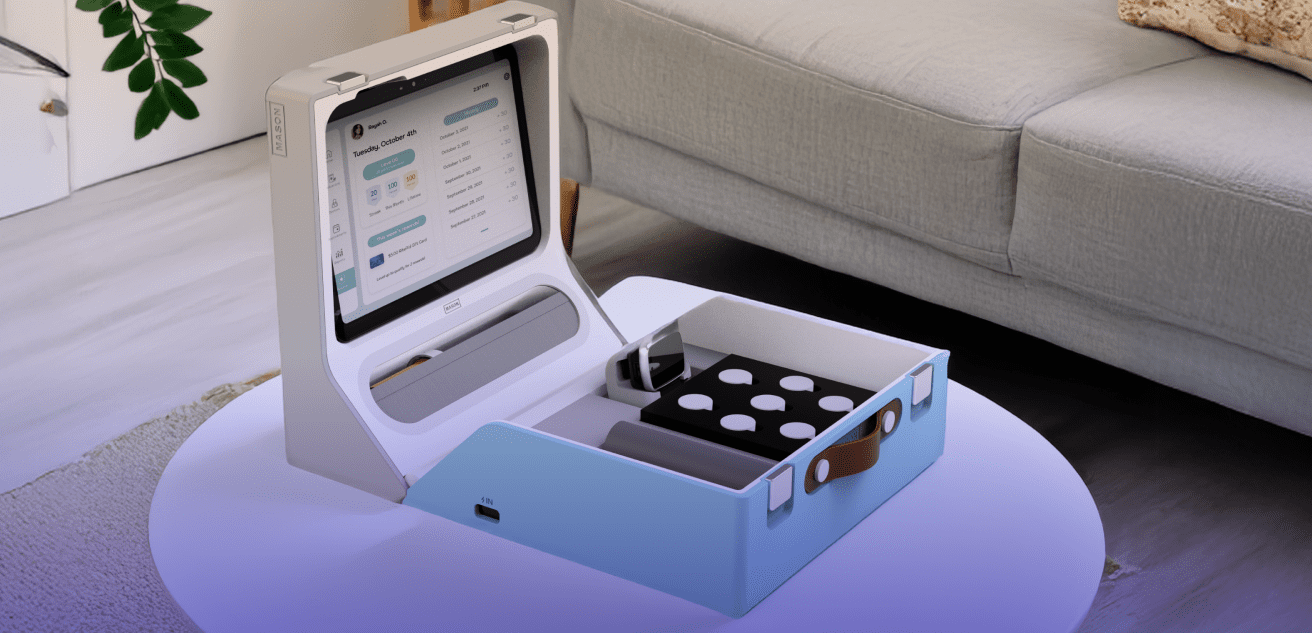
(Image: bymason.com)
When I designed Mason’s RPM kit, I asked myself, “What can I do to make it extra beneficial for its users?”
I wanted to create a system that brings the hospital to patients’ homes, not vice versa. Mason’s RPM kits can empower patients and providers, giving them an experience that transcends bureaucracy and focuses on well-being.
To make it happen, I knew that the kit’s ecosystem—from hardware to software and connectivity—must work seamlessly. I realized it needs to combine cutting-edge technology with an unwavering focus on usability and efficiency.
And I’m glad it did.
Our remote monitoring kits are designed to provide hospital-grade accuracy while remaining simple enough for everyday use. From its advanced sensors that capture critical health data to the incorporation of the groundbreaking Bluetooth Low Energy (BLE), the RPM kit enables patients to interact with devices as effortlessly as possible with a smartphone.
As a Staff Android Engineer leading this project, I ensured that the BLE connectivity framework not only works well with devices but also on an enterprise-level provides the same level of confidence. This framework enabled Mason to develop the first fully customizable solution for patient monitoring in hospitals and medical institutions, improving patient care outcomes while maintaining quality, real-time data.
Furthermore, Mason’s kits boast seamless hardware and software. Built on a customizable Android-based framework, they integrate seamlessly with various medical peripherals using standardized APIs. By architecting and deploying custom Android apps with the BLE framework, we enabled seamless pre-configuration with any medical peripherals—pulse oximeters, glucose meters, and even heart rate monitors. Our software allowed developers to access detailed metadata to ensure compatibility across multiple devices, redefining what it means to be tech-savvy in the medical landscape.
Additionally, our kits use real-time visualization and automated alerts to notify providers of changes in patient vitals. This way, they know what’s happening to the patient, whether their condition improves or worsens.
The kit also supports over-the-air updates to ensure security without needing physical replacements.
And its improvements continue beyond that.
We ensured patients in rural or underserved areas could still use the RPM kit. We engineered the devices to operate over cellular networks, reducing reliance on Wi-Fi and ensuring accessibility in diverse settings. We also implemented end-to-end encryption to secure patient information throughout the transmission process. This feature ensures we adhere to relevant regulations, like HIPAA and GDPR, while maintaining a high quality of patient service.
However, perhaps the most rewarding part of building Mason’s RPM kits was making them accessible to patients regardless of their technical skills.
While building the kit, I thought long and hard—how can I make it easy for patients (and their families) to use?
And my answer lies in its intuitive and empowering interface.
The RPM kit allows patients to interact with the system via a touch-screen interface, guiding them through each step. This intuitive interface eliminates the technical stuff that burdens patients and focuses on what matters—monitoring their health.
By integrating these groundbreaking technologies into RPM kits and handheld devices such as smartwatches, Mason created a robust solution that streamlines setup, reduces errors, and improves patient outcomes—a complete win for patients and medical professionals everywhere. The Mason A4100 smartwatch replaced traditional ankle-based monitoring, allowing patients to feel empowered and dignified when it comes to getting better.
And with the success of developing these devices comes a venture like no other—our kits and mobile devices have been successfully deployed in clinical trials across the US. By partnering with the Vial Contract Research Organization (CRO), we can accelerate the development of new therapies and make the entire process more straightforward and patient-centered.
Our RPM kits represent a new frontier in healthcare—where technology actively drives care. We’ve managed to break down the complexities of RPM into an integrated, inclusive, and user-focused solution, helping patients manage their well-being independently and confidently.
Healthcare Technology Solutions for a More Independent and Confident Patient of Tomorrow
The Mason RPM kit is just one example of how smart devices revolutionize healthcare. Whether it’s ECG monitors that patients can wear to AI-powered diagnostic tools, I’m sure there’s more to the future of digital health.
However, its goal remains the same—making healthcare proactive and patient-centric to improve their quality of life.
And the same goes for me.
I believe that the future of healthcare will be far better than it is now. I aim for a tomorrow where we don’t go to the hospitals for check-ups and treatments, only for emergencies. I want to empower people to confidently take control of their health, whether they are rich or poor, with health conditions or without.
And to realize this future, innovative healthcare isn’t enough—it also needs to be more humane. As engineers in the healthcare sector, we must always ask how technology can make healthcare accessible.
We must remember that the innovations we’re building today are laying the foundation for the future of healthcare—one in which providers and patients are empowered and confident.
About the Author
Kaushlendra Tripathi is a seasoned Lead Android Engineer designing innovative and scalable solutions for various industries. His dedication to improving the quality of life using technology led him to specialize in user-centric platforms that integrate cutting-edge hardware and software. His innovative mindset allowed him to pioneer groundbreaking technologies that reshape how medical professionals approach patient care, emphasizing his belief that technology and life can mesh together with transformative and functional solutions.
Resources:
Esteva, A., Robicquet, A., Ramsundar, B., Kuleshov, V., DePristo, M., Chou, K., Cui, C., Corrado, G. S., Thrun, S., & Dean, J. (2019). A guide to deep learning in healthcare. Nature Medicine, 25(1), 24-29. https://doi.org/10.1038/s41591-018-0316-z
Fagherazzi, G., Goetzinger, C., Rashid, M. A., Aguayo, G. A., & Huiart, L. (2020). Digital health strategies to fight COVID-19 worldwide: Challenges, recommendations, and a call for papers. Journal of Medical Internet Research, 22(6), e19284. https://doi.org/10.2196/19284
JMIR Publications. (2020). Digital health: Trends and innovations in healthcare technology. https://www.jmir.org/2020/11/e20135/
Keesara, S., Jonas, A., & Schulman, K. (2020). Covid-19 and health care’s digital revolution. New England Journal of Medicine, 382(23), e82. https://doi.org/10.1056/NEJMp2005835
Khan, Y., Ostfeld, A. E., Lochner, C. M., Pierre, A., & Arias, A. C. (2017). Monitoring of vital signs with flexible and wearable medical devices. Annual Review of Biomedical Engineering, 19(1), 145-187. https://doi.org/10.1146/annurev-bioeng-071516-044506
Lin, M. H., Yuan, W. L., Huang, T. C., Zhang, H. F., Mai, C., & Wang, J. F. (2021). The impact of the COVID-19 pandemic on telemedicine and remote patient monitoring adoption: A systematic review. Telemedicine and e-Health, 27(10), 1027-1035. https://doi.org/10.1089/tmj.2020.0367
Liu, Y., Zhang, L., Yang, Y., & Li, G. (2022). Bluetooth Low Energy vulnerabilities in medical devices: A security perspective. Sensors, 22(21), 8280. https://doi.org/10.3390/s22218280
Reddy, S., Fox, J., & Purohit, M. P. (2019). Artificial intelligence-enabled healthcare delivery. Journal of the Royal Society of Medicine, 112(1), 22-28. https://doi.org/10.1177/0141076818815510
Smith, A. C., Thomas, E., Snoswell, C. L., Haydon, H., Mehrotra, A., Clemensen, J., & Caffery, L. J. (2020). Telehealth for global emergencies: Implications for COVID-19. Frontiers in Digital Health, 2, 7. https://doi.org/10.3389/fdgth.2020.00007