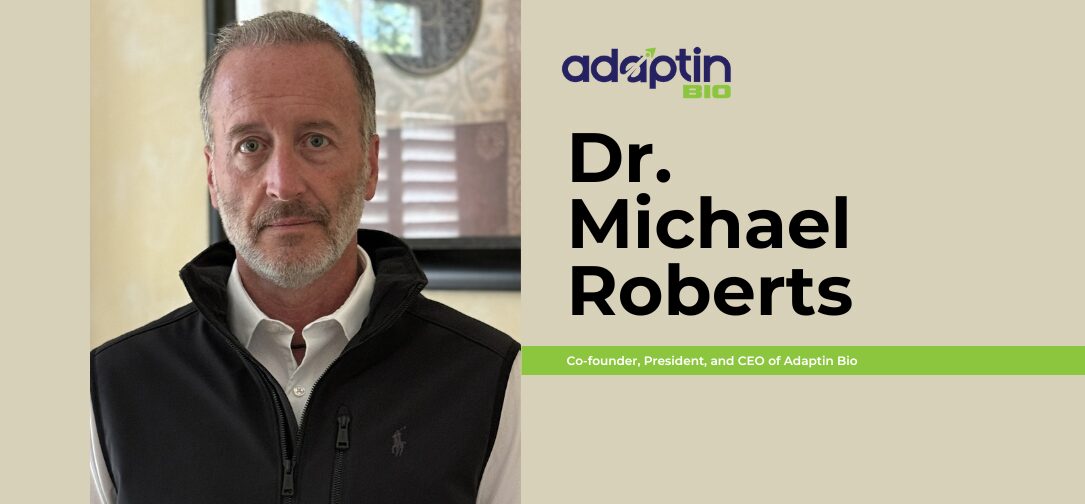
The blood-brain barrier (BBB) has long stood as one of the greatest challenges in medicine, thwarting efforts to deliver therapeutics to the brain and leaving many neurological conditions with few effective treatment options. But what if the solution wasn’t to break through the barrier, but to work with the body’s own systems to navigate it? In this in-depth TechBullion interview, we speak with Dr Michael J. Roberts, co-founder, President, and CEO of Adaptin Bio, whose pioneering BRiTE platform reimagines CNS drug delivery by enlisting the immune system itself. With a background spanning over two decades in pharmaceutical R&D, biotech leadership, and strategic deal-making, Dr Roberts is no stranger to innovation. He shares how Adaptin Bio is leveraging T cell biology to “hitchhike” therapies across the BBB, offering a promising new frontier not only for brain cancer, but also for neurodegenerative and neuroinflammatory diseases. From glioblastoma to gene therapy, this is a story about turning biological complexity into therapeutic opportunity, and redefining what’s possible in brain-targeted medicine.
1) Please tell us more about yourself.
Michael J. Roberts, Ph.D.
I’m a scientist, entrepreneur, and biotech executive with over 25 years of experience spanning pharmaceutical R&D, business development, and company building. I currently serve as the co-founder, President, and CEO of Adaptin Bio, where I’m focused on advancing novel therapeutics to address complex, often underserved diseases. I also sit on our Board of Directors.
Before founding Adaptin, I co-founded and served as CEO of Corino Therapeutics, where I led all aspects of the company’s strategy and operations. There, I directed the development of CRX-1008, a disease-modifying therapy for transthyretin amyloidosis, a debilitating protein misfolding disorder.
In addition to my executive roles, I founded MAC B Consulting, where I advise pharmaceutical and biotech companies on R&D strategy, licensing, and corporate growth. Earlier in my career, I was Vice President of Business Development and a Corporate Officer at Chelsea Therapeutics, a public biotech company. I led business development and M&A efforts, culminating in Chelsea’s acquisition by H. Lundbeck A/S for $658 million.
Prior to Chelsea, I directed business development efforts at Nektar Therapeutics, working on transactions involving their Molecule Engineering platform with both major and specialty pharmaceutical partners. Throughout my career, I’ve helped drive deals and partnerships valued at over $1 billion.
I began my journey in drug development at Shearwater Corporation, where I led biopharmaceutical research and helped guide early-stage candidates through to Phase I studies. I was also one of the inventors of Movantik™, a treatment for opioid-induced constipation later licensed to AstraZeneca in a deal valued at $1 billion. Shearwater was acquired by Inhale Therapeutic Systems (now Nektar) for $200 million.
I hold a Ph.D. in Materials Science from the University of Alabama and a B.S. in Chemical Engineering from Penn State. My work has always been driven by a passion for translating science into impactful therapies—and building the teams and partnerships to make that possible.
2) The blood-brain barrier has long posed a major obstacle to treating brain diseases. Can you describe why this barrier is so impenetrable and what makes it such a significant challenge for drug delivery?
The blood-brain barrier (BBB) is a highly specialized, selectively permeable interface in the capillaries in the brain that regulates the exchange of substances between the systemic circulation and the central nervous system (CNS). It is composed primarily of endothelial cells connected by tight junctions, supported by pericytes, astrocytic end-feet, and a basement membrane. These structural features create a physical and biochemical barrier that severely restricts the passive diffusion of most solutes, including over 98% of small-molecule drugs and nearly all macromolecular therapeutics such as peptides, proteins, and nucleic acids.
The BBB’s impermeability is further reinforced by active efflux transporters, such as P-glycoprotein, which actively expel xenobiotics and many pharmacological agents from the CNS back into the bloodstream. Moreover, the absence of fenestrations and low rates of transcytosis limit paracellular and vesicular transport, respectively. While essential for maintaining CNS homeostasis and protecting neural tissue from toxins and pathogens, this barrier presents a significant obstacle to the delivery of therapeutic agents intended to treat neurological diseases.
Consequently, drug development for CNS disorders, such as glioblastoma (GBM), Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS), is profoundly constrained by the BBB. Systemic delivery methods often fail to achieve therapeutic concentrations in the brain, and invasive approaches (e.g., intracerebral or intrathecal administration) carry procedural risks and limited applicability. As such, overcoming the BBB, either through molecular engineering of therapeutics, temporary modulation of barrier permeability, or utilization of carrier-mediated and receptor-mediated transport mechanisms, remains a central focus of translational neuroscience and pharmaceutical research.
3) Adaptin Bio’s BRiTE platform leverages the immune system for drug delivery. Could you walk us through how this technology works and what makes it different from other blood-brain barrier penetration strategies?
Adaptin Bio’s BRiTE (Brain Bispecific T Cell Engager) platform offers a novel strategy for delivering therapeutics across the BBB, a longstanding obstacle in the treatment of CNS disorders. Rather than relying on passive diffusion, transcytosis, or mechanical disruption, the BRiTE platform leverages endogenous immune cell trafficking mechanisms to enable targeted, efficient, and repeatable delivery of therapeutic agents to the brain.
The BRiTE platform is designed to exploit the natural capacity of activated immune cells, particularly T lymphocytes, to traverse the BBB during physiological immune surveillance and in response to neuroinflammatory signals. Adaptin’s proprietary approach involves utilizing functionalized therapeutic payloads, which may include small molecules, proteins, nucleic acids, or gene-editing constructs, with ligands or molecular tags that selectively bind to cell surface markers or receptors expressed on these CNS-trafficking immune cells. Our initial payloads focus on the use of T cell engagers that bind CD3 receptors on T cells.
The BRiTE process is a multi-step, highly controlled procedure that begins with the collection of the patient’s T cells and ends with the infusion of a bispecific T cell engager and manipulated T cells. The patient undergoes a procedure called leukapheresis, where blood is withdrawn, white blood cells (including T cells) are separated, and the remaining blood is returned to the body. T cells are then enriched from the leukapheresis product and manipulated to express certain surface receptors and adhesion molecules. These T cells are then expanded to obtain sufficient numbers for systemic therapeutic dosing.
The payload and manipulated T cells associate in circulation following their systemic administration. As these cells migrate across the BBB, driven by chemotactic signals or antigenic cues, the associated therapeutic cargo is co-transported into the CNS. Once localized within brain parenchyma or perivascular compartments, the platform enables the release of the therapeutic payload or activates the T cell, in the case of T cell engagers, upon binding to a tumor cell.
Unlike traditional strategies such as receptor-mediated transcytosis (e.g., via transferrin or insulin receptors) or temporary BBB disruption (e.g., via focused ultrasound or osmotic agents), BRiTE does not require alteration of BBB permeability or extensive molecular re-engineering of the drug itself. Its key differentiators include:
- Physiological compatibility: By co-opting immune cell trafficking rather than bypassing or compromising the BBB, BRiTE maintains barrier integrity and minimizes off-target CNS exposure.
- Modality flexibility: The platform is compatible with a broad range of therapeutics, including biologics and nucleic acid-based therapies, which typically face significant BBB delivery limitations.
- Repeat dosing potential: Because BRiTE aligns with normal immune physiology, it may enable chronic or repeated administration without inducing immune exhaustion or barrier disruption.
The BRiTE platform represents a paradigm shift in CNS drug delivery, transforming immune surveillance from a biological barrier into a transport vector, and enabling the development of novel therapeutics for previously inaccessible neurological targets.
4) The concept of “hitchhiking” on immune cells is both novel and elegant. What inspired this approach, and what were the key scientific or technical breakthroughs that made it possible?
The concept of “hitchhiking” on immune cells, central to Adaptin’s BRiTE platform, was inspired by a convergence of insights from immunology, neurobiology, and drug delivery science. The core idea emerged from observations that certain immune cells, particularly activated T cells, are among the few cell types that can routinely traverse the BBB, especially during episodes of neuroinflammation or immune surveillance. These cells possess surface receptors and adhesion molecules (e.g., LFA-1, VLA-4, CCR5) that allow them to engage with endothelial cells and extravasate into the CNS, a capability that most therapeutic agents lack.
The inspiration for the BRiTE approach stemmed from the question: If the immune system already has a built-in, regulated pathway for accessing the brain, could we co-opt this for therapeutic delivery? Researchers at Duke University under the direction of Dr. John Sampson, the former Robert H. and Gloria Wilkins Distinguished Professor and Chair of the Department of Neurosurgery at Duke University and currently Dean and Vice Chancellor at the University of Colorado School of Medicine, recognized that therapeutic agents could be designed to associate with these trafficking immune cells, effectively “hitchhiking” across the BBB by leveraging the cells’ natural homing and migration machinery. This bypasses the need to force entry through passive diffusion or mechanical disruption, offering a biologically elegant and targeted solution.
Several scientific and technical advances converged to make this strategy feasible:
- Characterization of immune cell trafficking into the CNS: Advances in immuno-neurology clarified how T cells home to sites of CNS injury or inflammation, including the molecular signals and adhesion cascades involved in their extravasation across the BBB.
- Surface engineering and targeting ligands: Progress in protein engineering has allowed the development of ligands or conjugates that can selectively bind to immune cell surface markers without impairing cell function, enabling associations between therapeutic cargo and trafficking cells.
- In vivo imaging and tracking tools: High-resolution imaging and immune cell tracking in animal models helped confirm that hitchhiking cargo could cross the BBB and accumulate in relevant CNS tissues, validating the biological transport mechanism and informing dosing and optimization.
- Understanding of disease-specific neuroinflammation: Knowing that many CNS diseases, including glioblastoma, are accompanied by localized immune cell infiltration allowed for disease-targeted applications, maximizing both specificity and therapeutic index.
The BRiTE platform was made possible by rethinking the BBB not as an insurmountable barrier, but as a dynamic interface that could be navigated using the body’s own cellular infrastructure. It represents a shift from brute-force delivery methods to precision-guided biological integration, a direction with profound implications for treating CNS disorders.
5) Adaptin is targeting difficult-to-treat cancers, particularly glioblastoma. What makes glioblastoma an ideal candidate for BRiTE-based therapies, and how far along are you in preclinical or clinical development?
Glioblastoma is among the most treatment-resistant and immunologically complex cancers, due in large part to its immune-suppressive microenvironment, anatomical isolation behind the BBB, and extreme intratumoral heterogeneity. Adaptin’s BRiTE platform provides a novel strategy that directly addresses these challenges by using the body’s own immune trafficking mechanisms to deliver functional T cells and therapeutic payloads into the brain, offering a compelling and differentiated approach to GBM treatment.
A major barrier to immunotherapy in GBM is the presence of anergic or exhausted T cells within the tumor microenvironment (TME). Multiple immunosuppressive mechanisms, including chronic antigen stimulation, high expression of checkpoint ligands (e.g., PD-L1), immunosuppressive cytokines (e.g., TGF-β, IL-10), presence of immunosuppressive regulatory T cells, and nutrient competition, render infiltrating cytotoxic T cells dysfunctional and unable to sustain anti-tumor activity.
The BRiTE platform circumvents this by enabling the systemic delivery of functional and activated T cells that retain their cytotoxic capacity. T cell engagers “hitchhike” on these immune cells that are naturally capable of crossing the BBB, reaching the CNS in an active, unexhausted state, thus restoring the potential for effective immune engagement and killing of tumor cells via the T cell engager. The release of T cell engagers in the TME can convert the immunosuppressive role of regulatory T cells into a cytotoxic T cell against tumor cells.
BRiTE also overcomes tumor heterogeneity with modular payload delivery to a wide range of tumor targets. A defining feature of GBM is its high degree of spatial and molecular heterogeneity, with subpopulations of tumor cells expressing distinct antigen profiles and resistance mechanisms. This heterogeneity has limited the effectiveness of single- or double-target therapies (such as CAR T cells).
The BRiTE platform addresses this by enabling modular co-delivery of additional therapeutic payloads, including a) multiple T cell engagers that redirect T cells toward multiple tumor antigens and b) checkpoint inhibitors to locally reverse immune suppression. By delivering these components directly into the CNS alongside functional T cells, BRiTE provides a multi-pronged attack that can adapt to tumor evolution, target resistant populations, and reduce the likelihood of immune escape.
The BRiTE platform offers a solution to the key challenges of glioblastoma: it bypasses the BBB, restores functional immune engagement, enables modular and repeatable delivery, and addresses tumor heterogeneity with customizable payloads. For a disease where conventional and advanced therapies have consistently fallen short, BRiTE represents a fundamentally new and highly promising therapeutic paradigm.
6) Delivering potent therapies directly to the brain raises concerns about precision and safety. How does your platform ensure that therapeutics are not only delivered past the barrier but also correctly targeted to avoid off-site effects?
Delivering potent therapies to the brain requires an exceptionally high standard for precision, safety, and control, given the brain’s sensitivity and the irreversible consequences of off-target exposure. The BRiTE platform is specifically engineered to meet these demands through a multi-layered targeting strategy that ensures therapeutics are not only delivered across the BBB but also become active only at the intended disease sites, minimizing exposure to healthy tissue.
BRiTE incorporates T cell engaging payloads that restrict therapeutic activation to the site of interest. This includes the use of tumor specific antigen targeting and activation of T cell engaging payloads within the disease site or tumor microenvironment. These mechanisms ensure that even once across the BBB, therapeutic agents remain inert until they reach the pathological site, significantly improving safety margins.
The BRiTE platform is modular by design, allowing precise control over payload type and potency and activation locally. This level of tunability allows therapies to be customized for specific indications, dosing schedules, and patient safety profiles, offering greater control than conventional approaches.
BRiTE addresses the dual challenge of crossing the BBB and achieving precise delivery within the brain through an integrated strategy that couples cell-based targeting, controlled activation, and disease-specific homing. This provides not only unprecedented delivery efficiency but also a strong safety profile, essential for treating complex CNS diseases without compromising neural integrity.
7) While your current focus is brain cancers, does the BRiTE platform have potential applications beyond oncology, perhaps in neurodegenerative diseases like Alzheimer’s or Parkinson’s?
The BRiTE platform has broad potential that extends well beyond oncology. While brain cancers like glioblastoma are an urgent and high-need proving ground due to their aggressiveness and the limitations of current therapies, the core mechanism of BRiTE, immune cell–mediated, targeted delivery across the BBB, is highly applicable to a range of neurodegenerative and neuroinflammatory diseases, including Alzheimer’s disease, Parkinson’s disease, ALS, multiple sclerosis, and others.
Many neurodegenerative disorders are now recognized as involving chronic, low-grade neuroinflammation, characterized by the infiltration of immune cells (particularly monocytes and T cells) into specific brain regions. BRiTE is designed to exploit this localized immune trafficking, allowing therapeutics to hone in on precisely the areas where disease processes are most active.
Most current treatments for neurodegenerative diseases are symptomatic and small-molecule based, due to the inability of larger, disease-modifying biologics (e.g., antibodies, enzymes, oligonucleotides, or gene therapies) to cross the BBB. BRiTE can potentially overcome this delivery barrier and enable:
- Delivery of anti-amyloid or anti-tau antibodies in Alzheimer’s
- Gene therapies or RNA-based interventions in ALS or Huntington’s
- Neuroprotective proteins or anti-inflammatory agents in Parkinson’s
Neurodegenerative diseases are chronic and progressive, requiring long-term treatment regimens. Unlike invasive methods (e.g., intrathecal or intracerebral injection), BRiTE’s non-disruptive, immune-guided delivery supports repeat dosing and chronic administration, a key advantage for long-term disease management.
Because the BRiTE platform is payload-agnostic, it can be tailored to a wide array of therapeutic strategies, including immunomodulators to reduce neuroinflammation, neurotrophic factors to promote neuronal survival, and enzyme replacement therapies for lysosomal storage disorders. With neurodegenerative disorders being recognized as involving chronic, low-grade neuroinflammation, BRiTE has the capability of utilizing regulatory T cells as the delivery vehicle, thus providing an additional anti-inflammatory component.
While BRiTE is currently focused on brain cancers, its mechanistic foundation is broadly applicable across CNS diseases where immune trafficking can be harnessed for delivery. This includes major neurodegenerative diseases like Alzheimer’s and Parkinson’s, where the platform could enable disease-modifying therapies that are currently limited by delivery barriers. In the long term, BRiTE has the potential to transform how we approach the treatment of virtually any condition involving the brain, offering a powerful tool for targeted, efficient, and safe CNS drug delivery.
8) Lucius Partners has backed Adaptin as part of its life sciences portfolio. What do you think made your approach stand out to investors, and how has that partnership accelerated your progress?
Lucius Partners recognized in Adaptin, a rare convergence of scientific novelty, platform versatility, and clinical urgency. What likely stood out to them, and what continues to resonate with other sophisticated investors, is that our BRiTE platform isn’t just a drug or a delivery mechanism; it’s a fundamentally new modality for crossing the blood-brain barrier with precision and adaptability.
What differentiated Adaptin from the outset is our immunologically driven approach. While many BBB strategies rely on passive diffusion, invasive delivery, or receptor-mediated transcytosis, we use circulating immune cells, particularly T cells, as biological vectors to carry therapeutics directly to diseased areas of the brain. This “hitchhiking” method not only exploits the brain’s own inflammatory signals to localize delivery, but also enables modular payload attachment, including small molecules, proteins, gene therapies, and cell engagers. It’s that intersection of immunology, drug engineering, and CNS targeting that made our platform stand out in a crowded field.
Lucius also saw our strong executional track record. As a team, we’ve taken multiple programs from concept through clinical development and successful exits. That gave them confidence that we understood not only the science but also the critical path for value creation, including CMC, regulatory strategy, and partnering.
Their support has been catalytic. Lucius Partners brings more than capital, they bring deep operational insight, strategic connectivity, and biotech infrastructure support. Through them, we’ve accelerated our timeline on key IND-enabling activities and expanded our visibility among potential partners and collaborators.
The partnership has allowed us to move with speed and strategic clarity, while staying focused on our mission: to transform how therapies are delivered to, and act within the brain.
9) What are the key regulatory or commercial milestones you’re aiming for in the next 12–24 months, and what challenges do you anticipate in bringing this platform to market?
Over the next 12 to 24 months, our primary focus is on reaching a critical inflection point, both regulatory and clinical, that will validate the BRiTE platform and set the stage for a pathway to commercialization. These milestones are designed to de-risk the technology and establish a strong foundation for therapeutic development, strategic partnerships, and eventual market entry.
Our goal within the next 12 months is to initiate and execute on our first-in-human (FIH) study with our first product candidate, APTN-101 (EGFRviii x CD3 T cell engager). Establishing a pipeline of additional product candidates that target a variety of tumor antigens for enhanced therapeutic effect for treating brain tumors is a particular strategic focus.
We are also pursuing partnerships with biopharma companies that could leverage BRiTE for delivery of their own CNS-targeted assets. These collaborations would validate the modular and payload-agnostic nature of the platform while helping to de-risk commercial development. Additionally, we expect to expand and strengthen our patent estate, not only for the core BRiTE technology but also for specific payloads and disease applications. A strong IP position will be essential for long-term differentiation and value creation.
As with any novel delivery platform, BRiTE may face challenges from regulatory bodies, particularly around delivery dynamics, safety, reproducible manufacturing and quality control.
For a platform technology, selecting the right first indication and endpoints is vital. Glioblastoma presents an opportunity with an urgent need but also clinical complexity, including rapid disease progression, imaging-based response variability and heterogeneity in immune infiltration and tumor microenvironment.
The concept of immune-guided, cross-BBB delivery is novel and may require education of stakeholders, from clinicians to investors. Clear articulation of BRiTE’s advantages over traditional CNS delivery methods, such as receptor-mediated transcytosis, intrathecal administration, or viral vectors, will be key for market adoption.
Over the next two years, our goal is to de-risk and validate BRiTE through IND-enabling work, regulatory engagement, and early partnerships, paving the way for FIH studies. While we anticipate challenges around regulatory complexity, manufacturing, and clinical strategy, we believe the transformative potential of the platform, especially in the context of urgent, underserved CNS diseases, makes this effort both timely and highly impactful.
10) Looking 5 to 10 years ahead, how do you envision Adaptin Bio’s technology changing the landscape of treatment for brain-related diseases?
Looking 5 to 10 years ahead, I believe BRiTE technology has the potential to fundamentally reshape how we treat brain-related diseases; not just by improving drug delivery, but by redefining what’s possible in the development and deployment of CNS therapies.
Historically, the BBB has been viewed as an almost insurmountable blockade, responsible for the failure of countless promising therapies in neurology and oncology. BRiTE turns this paradigm on its head, transforming the BBB from a barrier into a selective gateway, using the body’s own immune cells as precision delivery vehicles. In the next decade, I see this strategy moving from the exception to the norm, particularly for therapies that were previously too large, fragile, complex to reach the CNS or the function of T cell subtypes are important.
BRiTE could open the door to entirely new therapeutic modalities for brain diseases, especially those that were previously untreatable or poorly managed. In conditions like glioblastoma, Alzheimer’s, Parkinson’s, ALS, and rare genetic or lysosomal storage disorders, BRiTE could make it feasible to deliver a range of therapeutic modalities. For glioblastoma in particular, BRiTE has the capability to transform a universally fatal disease into a disease that can be managed over many years.
The modular design of BRiTE makes it highly adaptable, not just to different diseases, but to individual patients. In the future, we could see customized BRiTE therapies, where the choice of immune cell type, therapeutic payload, and delivery timing is tailored to the patient’s specific disease profile, stage, and even brain region involvement. This could mark a major shift toward precision medicine in neurology and neuro-oncology, where treatments are dynamically adjusted based on imaging, biomarkers, and immune signatures.
Ultimately, I envision BRiTE becoming not just a delivery tool, but a platform standard, the backbone for a new generation of brain-directed therapies. It could be licensed by other drug developers, integrated into combination regimens, and used across indications, from oncology to neurodegeneration to neuroinflammation. In much the same way that lipid nanoparticles revolutionized mRNA delivery, BRiTE could revolutionize how we cross the BBB, safely, selectively, and repeatedly.