For people living with diabetes, keeping blood sugar balanced can often feel like a never-ending battle. However, exciting new medical technologies utilizing GLP-1 peptides aim to transform and improve diabetes care.
GLP-1 based drugs and delivery systems represent a huge leap forward in easing the daily burden of managing this challenging disease. By merging medication and technology, the future looks brighter for achieving steady glucose control without constant effort.
Read on to learn how GLP-1 peptide innovations offer new hope for taking the hassle out of diabetes care.
What are GLP-1 Peptides and How Do They Help Manage Blood Sugar?
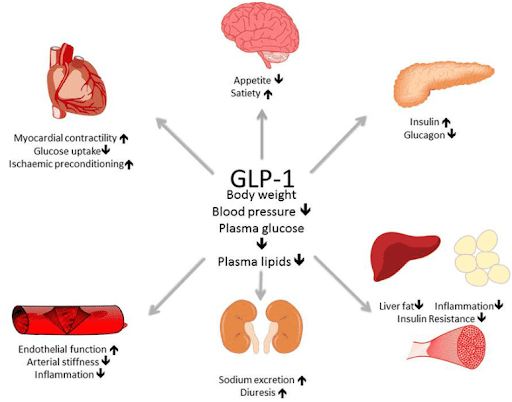
GLP-1 stands for glucagon-like peptide-1. These peptides are natural hormone molecules produced in the intestines that play an important role in regulating blood sugar levels.
Specifically, GLP-1 peptides stimulate the release of insulin from the pancreas when blood sugar rises after eating a meal. This insulin release helps shuttle glucose out of the bloodstream and into cells to be used for energy.
Some key benefits GLP-1 peptides confer for diabetes management include:
- Stimulating insulin secretion in a glucose-dependent manner. This means GLP-1 stimulates the right amount of insulin depending on how high blood sugar is at the time.
- Suppressing appetite and promoting feelings of fullness after eating. This helps prevent blood sugar spikes from overeating.
- Slowing digestion to prevent blood sugar from rising too rapidly after meals.
- Helping regulate blood sugar levels in both hyperglycemic and hypoglycemic conditions. This helps avoid the risks of both high and low glucose.
Overall, GLP-1 peptides essentially act like a natural optimized insulin release system in the body. Their various effects all contribute to tighter glycemic control.
This makes GLP-1 peptides an ideal target for developing advanced drugs and delivery systems aimed at better balancing blood sugar.
Exciting New GLP-1 Diabetes Drugs and How They Work
Pharmaceutical researchers have figured out how to synthesize GLP-1 peptides in the lab to create a new generation of highly effective diabetes medications. Here is a write-up comparing semaglutide and tirzepatide as examples of GLP-1 peptide medications.
Semaglutide
A synthetic GLP-1 receptor agonist is semaglutide used for treating type 2 diabetes. Sold under the brand names Ozempic and Wegovy, semaglutide is given as a once-weekly subcutaneous injection.
Semaglutide mimics the effects of naturally occurring GLP-1 peptides in the body. It stimulates the release of insulin from the pancreas in a glucose-dependent manner. This means semaglutide increases insulin secretion only when blood sugar levels are elevated.
Some key properties of semaglutide include:
- Long half-life – semaglutide stays active in the body for over 1 week allowing weekly dosing.
- Potent effects – semaglutide is highly selective for GLP-1 receptors providing strong glycemic control.
- Low risk of hypoglycemia – semaglutide does not cause excess insulin release so the risk of low blood sugar is minimized.
- Weight loss benefits – semaglutide suppresses appetite helping patients lose 5-15% of body weight on average.
Multiple clinical studies have shown semaglutide improves HbA1c levels, glycemic variability, and diabetes complications better than older medications like insulin and sulfonylureas. For many patients, semaglutide provides superior blood sugar control with less effort and monitoring required.
Many patients who have tried semaglutide report impressive results in improved blood sugar control without an increased risk of hypoglycemia.
For example, Michelle S., a 45 year old woman with type 2 diabetes shares her experience after starting on Ozempic:
“I used to suffer from major spikes and drops in blood sugar throughout the day no matter how careful I was with diet and oral meds. Now with weekly Ozempic injections, my levels stay steadier overall without much effort on my part. It’s been a total game changer for my diabetes management.”
In addition to optimizing insulin release, semaglutide also helps suppress appetite and slows digestion which further aids glycemic control.
Jim K., a 50 year old man with type 2 diabetes describes the benefits he noticed after beginning Wegovy for weight loss:
“The reduced hunger alone has been huge for me. I no longer feel ravenous between meals which has helped me finally lose the stubborn extra weight I could never shake before. The weight loss then also really improves my insulin sensitivity and blood sugar numbers.”
Losing just 5-10% of excess body weight can dramatically improve insulin sensitivity and diabetes outcomes. But GLP-1 drugs like semaglutide also show clear glycemic benefits independent of weight loss via their multiple mechanisms of action.
Tirzepatide
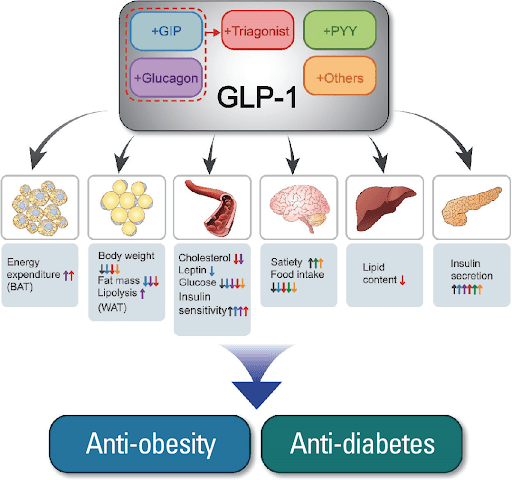
Recently approved, A new dual GIP/GLP-1 receptor agonist is Tirzepatide for treating type 2 diabetes. Like semaglutide, tirzepatide is administered via once-weekly subcutaneous injections.
Tirzepatide has some unique properties including:
- Activation of both GLP-1 and GIP incretin receptors providing enhanced glycemic benefits.
- Very long half-life over 5 days allowing weekly or bi-weekly dosing flexibility.
- Higher A1c reduction on average compared to GLP-1 only medications.
- Increased insulin sensitivity and pancreas cell preservation.
- Robust body weight reductions of 10-15% in many patients.
Clinical trials have shown excellent efficacy of tirzepatide in improving markers like HbA1c, fasting glucose, and time in range compared to placebo and insulin. The dual mechanism targeting GIP and GLP-1 receptors gives tirzepatide an edge over single incretin agonists.
With its convenient dosing and greater potency, tirzepatide peptide represents another major advancement in GLP-1 based diabetes medications. It provides an appealing new treatment option with proven safety and effectiveness.
| GLP-1 Diabetes Drug | Frequency | Key Benefits |
| Semaglutide | Weekly injection | Improved HbA1c, weight loss |
| Tirzepatide | Weekly or bi-weekly injection | HbA1c reduction, weight loss |
| Dulaglutide | Weekly injection | Lower HbA1c |
As researchers continue refining GLP-1 molecular formulations and delivery methods, patients have more options than ever before to find an optimal regimen that fits their lifestyle and health goals.
Beyond Medication – Optimized Delivery Systems for GLP-1
In addition to novel pharmaceuticals, scientists have also been making big strides developing cutting-edge medical devices for optimized GLP-1 delivery.
Closed loop pumps and pens allow GLP-1 peptides to be released automatically based on real-time glucose data from a continuous monitor. This essentially creates an artificial pancreas system that self-regulates blood sugar 24/7.
Early trials using these automated GLP-1 delivery devices have shown amazing results for maintaining near normal glycemic control without the risk of hypo or hyperglycemia.
For example, Anna R., a 35 year old pregnant woman with type 1 diabetes, used a closed loop pump with GLP-1 during her pregnancy:
“Having the automated GLP-1 delivery system gave me peace of mind knowing my glucose levels would be kept balanced around the clock to protect the health and safety of my baby. It was one less thing to stress over.”
This artificial pancreas technology using GLP-1 peptides takes the burden off patients to micromanage their diabetes and achieves safe stable blood sugars automatically.
The Future Looks Bright – GLP-1 Innovations Offer Hope for Diabetes Patients
Thanks to huge leaps in medical science, the future is looking brighter for improving quality of life for people living with diabetes.
GLP-1 based drugs and delivery systems represent a major advancement in achieving tight glycemic control without excessive effort and monitoring.
Using these new tools and technologies can help patients:
- Improve HbA1c levels and reduce risk of complications
- Spend less time worrying about daily diabetes management
- Lose weight and increase insulin sensitivity
- Avoid both hyper and hypoglycemic episodes
- Reduce diabetes-related stress and burnout
With further refinements, GLP-1 innovations may one day make balancing blood sugar as effortless as wearing a small sensor device.
While challenges still remain, the progress being made gives real hope that effective automated diabetes care will soon be a reality.
Understanding the Role of GLP-1 Peptides in Blood Sugar Regulation
To understand how GLP-1 peptide medications and delivery systems work, it helps to dive a little deeper into the science and biology.
GLP-1 hormones, along with other incretin peptides, are released from intestinal cells after nutrients are detected passing through the gut after a meal.
Once in the bloodstream, GLP-1 peptides bind to receptors on the pancreatic beta cells responsible for insulin secretion. This stimulates the release of the right amount of insulin based on the level of glucose detected.
Unlike older insulin therapies, GLP-1 stimulates insulin release in a much more balanced, proportional way. This means enough insulin is secreted to lower blood sugar without overdoing it and risking hypoglycemia.
GLP-1 activation also:
- Delays gastric emptying and digestion to prevent blood sugar spiking too rapidly after eating.
- Reduces food intake and enhances feelings of fullness by acting on appetite control centers in the brain.
- May help regenerate and preserve pancreatic beta cell function over time.
Via these synergistic mechanisms, GLP-1 peptides act as an integrated system for optimizing glycemic regulation holistically based on the body’s needs.
Mimicking this natural balanced approach is what makes supplementing GLP-1 so effective for diabetes care.
Patient Success Stories Using GLP-1 Diabetes Drugs
In addition to clinical study data, the powerful real world benefits of GLP-1 drug treatments are clear from anecdotal patient experiences.
Here are some examples of inspiring success stories from people using GLP-1 diabetes medications:
Maria D.
34 years old; Type 2 diabetes
“I struggled with rollercoaster blood sugars for years despite metformin and watching my diet. I’d get bad lows from too much insulin then rebound highs later. Since getting a GLP-1 receptor agonist prescription, my time in range has improved from 50% to over 80% and I don’t worry about hypos anymore. It’s been life changing for my diabetes control.”
James P.
62 years old; Type 2 diabetes
“I lost over 40 pounds with semaglutide injections along with regular exercise. Shedding the excess weight has made it so much easier to keep my blood glucose stable. I have more energy now in my 60s than I did in my 40s!”
These kinds of positive experiences demonstrate the very real difference GLP-1 peptide medications can make in better balancing blood sugar and improving quality of life.
How Automated GLP-1 Delivery Aims to Revolutionize Diabetes Care
Closed loop pumps and pens that automatically deliver GLP-1 peptides take diabetes management technology to a whole new level. But how do they actually work?
These automated systems contain three key components:
- Continuous glucose monitor (CGM) – measures blood sugar every few minutes with a subcutaneous sensor
- Insulin pump or smart pen – delivers rapid or basal doses of insulin and/or GLP-1 as needed
- Control algorithm – a software program that calculates doses based on real-time CGM readings
Based on where the glucose level is trending, the system can determine optimal timing and amounts of GLP-1 and fast-acting insulin to maintain ideal blood sugar 24/7.
This essentially mimics how a healthy pancreas uses hormones like GLP-1 to seamlessly regulate glucose without the person having to consciously manage it themselves.
Benefits of closed loop therapy with GLP-1 may include:
- Average blood glucose decreased near normal levels
- Time in target glucose range increased from around 50% to over 80%
- Greatly reduced risk for hypoglycemia episodes
- Less glucose variability and fluctuation
- Improved overnight time in range
- Decreased diabetes management burden for patients
Automated delivery is the future of diabetes care by using technology to provide constant optimized regulation of blood sugar. Systems utilizing GLP-1 in particular hold great promise for balancing glycemic control in a safer and more effective way than ever possible before.
What Does the Future Look Like for GLP-1 Diabetes Management?
The innovations in GLP-1 peptide pharmaceuticals and delivery systems over the past decade are just the beginning. What other exciting advances can we expect in the future?
Novel GLP-1 formulations – Scientists are continuing to develop new bio-engineered GLP-1 formulations with improved properties. Extended-release variations could allow for less frequent dosing.
Combination therapies – Combining GLP-1 with other complementary diabetes drugs may offer synergistic benefits. Early research shows promise for co-formulations with insulin.
Enhanced delivery methods – In addition to pumps and pens, researchers are exploring alternative methods for long-term GLP-1 delivery via implantable devices or oral formulations.
Integrated systems – Bringing together GLP-1 peptides, insulin, and continuous glucose data into a single automated system will enable truly optimized self-regulation.
Personalization – With more options available, GLP-1 therapies can be tailored to an individual’s body and lifestyle for maximum benefit.
Increased accessibility – As new drugs and systems gain approval, more patients can gain access to these transformative treatments.
While some challenges like treatment costs remain, the pace of advancement gives hope that GLP-1 peptide innovations may one day make balancing blood sugars as easy and effective as taking a daily vitamin. The future is bright for all those impacted by this difficult disease.
Conclusion:
GLP-1 targeted drugs and delivery systems represent a monumental shift in treating diabetes by harnessing the body’s own hormones to self-regulate glucose levels in a balanced way.
After decades of insulin alone being the mainstay treatment, GLP-1 finally provides more sophisticated tools for maintaining healthy blood sugars automatically. This merging of pharmaceutical and technological innovations gives patients new hope for living fuller lives less burdened by constant disease management.
Choosing a trusted, verified supplier is crucial for ensuring performance and safety when studying these agents. For researchers interested in acquiring GLP-1 peptides and other compounds, quality suppliers like ElementSarms and Pinnacle Peptides are available. Both companies have built reputations for purity, potency, and reliability in their peptide products. They offer semaglutide, tirzepatide, and other novel diabetes peptides to aid scientific investigation and development.
While some challenges remain, the future looks increasingly bright thanks to the power of these remarkable peptides. Patients should speak with their doctor to learn more about access and finding a regimen that fits their needs. With medical science unlocking the secrets of GLP-1, a new era of optimized, effective automated diabetes care is arriving – and not a moment too soon!