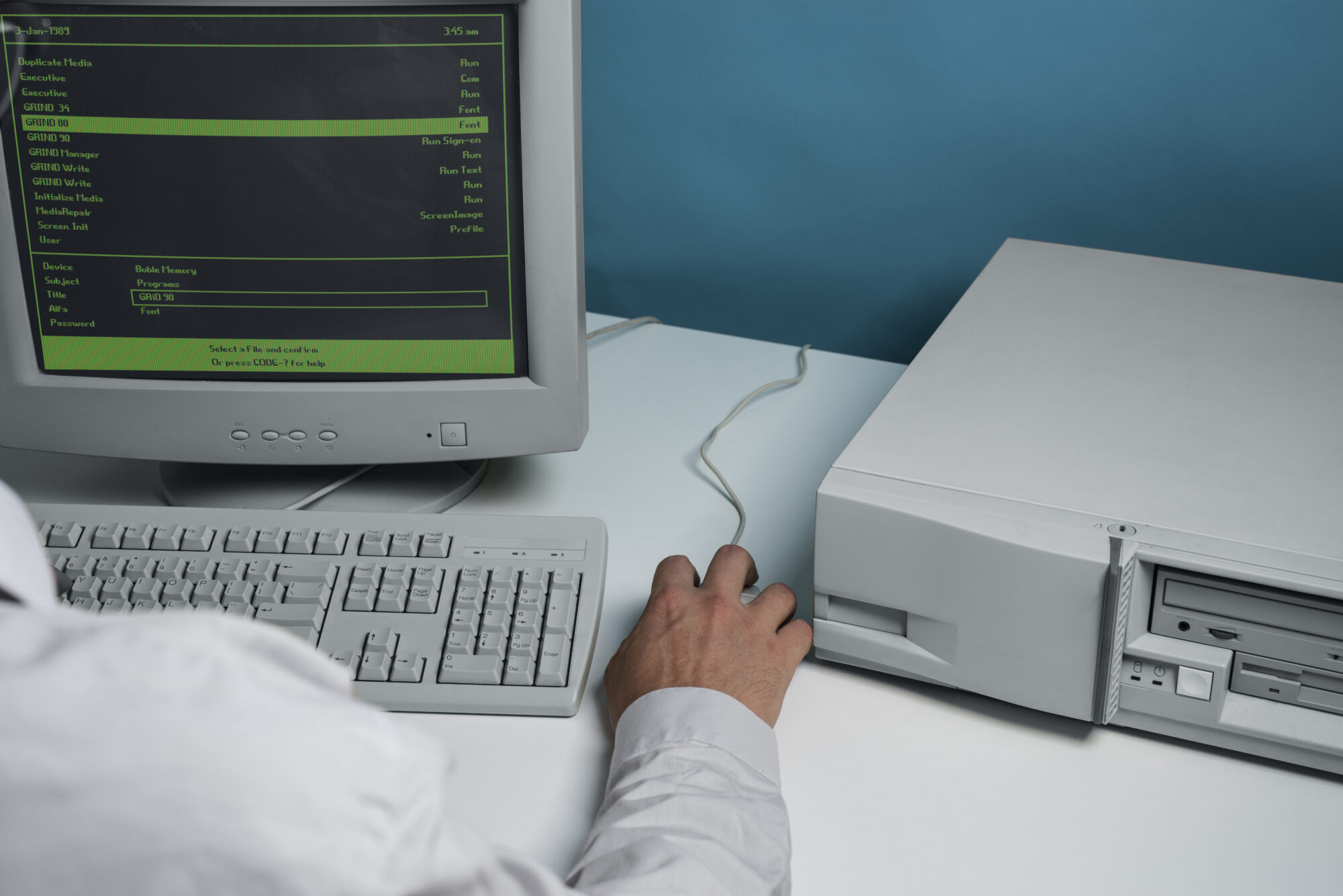
As medical devices become more connected, the risk of cyber threats rises. But when should developers begin thinking about cybersecurity? The answer is earlier than most expect, during design, not after deployment.
Imagine a wireless insulin pump that communicates with a smartphone app. If encryption protocols are not defined in the earliest stages of development, even a well-functioning device may carry hidden vulnerabilities. In a hospital setting, where multiple devices connect to shared networks, a single weak link can compromise not only data privacy but also patient safety.
Treating security as a technical add-on late in the process is no longer sufficient. It must be woven into the development lifecycle, guided by clear frameworks and reinforced by good engineering practice.
Recognizing the Stakes of Insecure Software
Medical device software does more than run diagnostics or record data. It often plays a direct role in clinical decisions and patient treatment. What happens if this software is compromised?
A malicious actor could manipulate therapy settings, alter vital sign readings, or interrupt data transmission. While these scenarios may sound extreme, the increasing complexity and connectivity of medical systems make them plausible. The consequences are not limited to data breaches; they extend to treatment delays, misdiagnoses, or life-threatening device behavior.
Understanding these stakes changes how teams view software security. It is not a matter of protecting code, it is a matter of protecting patients.
Where Design Decisions Influence Security Outcomes
Security is not something that can be retrofitted. Design-stage decisions set the tone for what a system can and cannot defend against. But what kinds of decisions are we talking about?
Take the example of user authentication. If a developer chooses to allow open access to software controls in the name of convenience, that decision becomes a security liability. If the software is designed to store patient data locally without encryption, that choice opens the door to data theft.
By considering potential threats during initial planning, before any code is written, developers can choose safer architectures, implement access controls, and define data handling policies that align with clinical use while minimizing risk.
How IEC 62304 Supports Secure-by-Design Development
So where does a structured framework come in? This is where IEC 62304 plays a vital role.
IEC 62304 is an international standard for the lifecycle processes of medical device software. While not exclusively focused on cybersecurity, it provides a foundation for building secure systems by requiring clear documentation, traceability, and verification at each development phase.
For example, the standard requires teams to define software safety classifications, Class A, B, or C, based on potential harm. Devices in the higher categories naturally face stricter requirements. Why does this matter for cybersecurity? Because these classifications inform the depth of threat modeling and control mechanisms required. A Class C device that delivers medication or controls critical life support functions will demand far more stringent security measures than a Class A tool used for non-critical logging.
IEC 62304 also emphasizes configuration management and change control. This ensures that once a secure state is established, it is not accidentally lost through careless updates or inconsistent practices. In this way, the standard helps developers embed security not just in the design but across the entire lifecycle.
Linking Cybersecurity to Risk Management
Cybersecurity is fundamentally about managing risk. But how can software developers in healthcare translate security concerns into actionable design choices?
The key lies in structured risk analysis. Teams must identify what threats exist, how likely they are to occur, and what the potential consequences would be. This analysis informs the selection of controls, such as user authentication, data encryption, input validation, and audit logging.
Consider a remote monitoring system that transmits patient vitals to clinicians via a cloud platform. Without proper threat assessment, developers may overlook risks like man-in-the-middle attacks or weak API authentication. By incorporating cybersecurity risks into the same risk management process used for clinical safety, developers avoid silos and ensure that all risks, digital or physical, are addressed with the same discipline.
The Role of Development Teams in Securing Medical Devices
Securing a device is not just the job of one person or one department. It requires coordinated action across development, quality assurance, regulatory, and clinical teams. But how can everyone stay aligned?
Good communication is essential. Developers must document how each requirement supports safety and security. Quality teams must verify that controls are tested and effective. Regulatory experts must ensure the approach aligns with FDA guidance or MDR expectations. When teams work from a shared understanding, they can build devices that not only perform their intended function but also defend against evolving threats.
Even seemingly small choices, like selecting a third-party library or using a default password during testing, can affect the system’s overall risk profile. That’s why secure thinking must be embedded in daily decisions, not reserved for compliance reviews or security checklists.
Looking Ahead: Future-Proofing with Security in Mind
The cybersecurity landscape will continue to shift. New vulnerabilities will emerge, and older devices may fall behind unless they are designed to evolve. So what can teams do today to prepare for tomorrow?
It starts with flexibility. Devices should be built with secure update mechanisms, allowing software to be patched or upgraded without introducing new risks. Monitoring systems should be capable of logging anomalies or suspicious behavior. And design documentation should be kept current, so new team members can understand past decisions and build upon them responsibly.
The goal is not just to pass audits or achieve certification. It is to create systems that earn and retain the trust of those who use them, because trust is what ultimately determines whether a device becomes part of clinical practice.
Conclusion: Building Security from the First Line of Code
Cybersecurity in medical device software is not about reacting to problems. It is about anticipating them and designing systems that are resilient by nature. By taking security seriously from the start, developers can build products that not only meet functional needs but also stand up to scrutiny from regulators, hospitals, and most importantly, patients.
IEC 62304 offers the structure to guide this effort, but it is up to each team to put the principles into practice. Secure-by-design is no longer optional. It is the standard that separates a promising device from one that can truly be trusted in the moments that matter most.