Prostate cancer, one of the most common malignancies affecting men worldwide, often presents a unique clinical challenge. Its typically slow-growing nature has led to the adoption of active surveillance as a viable management strategy for many patients. This approach, focused on monitoring rather than immediate treatment, hinges critically on the initial and ongoing assessment of cancer aggressiveness. Central to this evaluation is the prostate biopsy, a procedure that provides essential histological data, guiding clinicians in distinguishing between cases that require immediate intervention and those amenable to surveillance.
Prominent pathologist, Dr. Jonathan I. Epstein, explores the pivotal role of prostate biopsy in the decision-making process for active surveillance. With his wealth of experience and vast resume, Dr. Epstein lends valuable insight to examining various facets of prostate cancer identification and surveillance, including biopsy techniques, interpretation of results, and their implications for patient outcomes.
Understanding Prostate Biopsy: Techniques and Risks
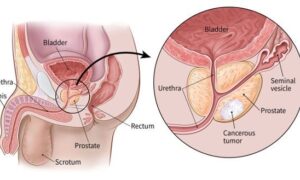
A prostate biopsy is a critical diagnostic tool in the detection and management of prostate cancer. It involves the extraction of small tissue samples from the prostate gland for microscopic examination. The techniques primarily used are Transrectal Ultrasound (TRUS)-guided biopsy and Magnetic Resonance Imaging (MRI)-guided biopsy.
“The TRUS-guided biopsy is the conventional method,” says Dr. Jonathan I. Epstein. “It employs ultrasound to visualize the prostate and guide needle insertion for tissue sampling.”
While effective, its limitation lies in the potential for missing small or atypically located tumors, as it relies on a systematic, rather than targeted, approach. In contrast, MRI-guided biopsy, a more recent innovation, utilizes MRI scans to identify specific areas within the prostate that appear suspicious.
This method allows for a more targeted approach, potentially increasing the accuracy in detecting clinically significant cancers. Fusion biopsy, which combines MRI and TRUS, is also gaining popularity. It merges MRI images with real-time ultrasound for a more precise biopsy.
Despite the critical role of these procedures, prostate biopsies are not without risks. Common complications include bleeding, infection, and discomfort. More severe, but less common, risks involve urinary retention and sepsis. The procedure can also lead to temporary erectile dysfunction and psychological distress.
The Role of Biomarkers and Genetic Testing
Biomarkers and genetic testing have increasingly become integral components in the landscape of prostate cancer diagnosis and management, complementing traditional methods like biopsy. These advanced tools offer a nuanced understanding of the disease, aiding in more personalized treatment strategies.
Notes Dr. Jonathan I. Epstein, “Key biomarkers in prostate cancer include Prostate-Specific Antigen (PSA) levels, Prostate Health Index (PHI), and the 4Kscore test.”
PSA, a protein produced by prostate cells, is the most commonly used biomarker. Elevated levels can indicate prostate cancer, but they can also be influenced by other factors like age, race, and prostate size. The PHI combines PSA, free-PSA, and [-2]proPSA levels, offering improved specificity in detecting prostate cancer and reducing unnecessary biopsies. The 4Kscore test goes a step further by integrating four kallikrein protein levels along with clinical information, providing a predictive score for the likelihood of high-grade prostate cancer.
The emerging role of genetic testing in prostate cancer is significant. It involves analyzing the patient’s DNA to identify inherited genetic mutations that might increase the risk of developing prostate cancer. Tests like BRCA1/2 or DNA mismatch repair genes can not only help in understanding familial risk but also influence treatment decisions. For instance, patients with certain genetic mutations might respond better to specific types of therapies, such as PARP inhibitors.
These biomarkers and genetic tests serve as valuable adjuncts to biopsy findings. While a biopsy provides direct evidence of cancer presence and its aggressiveness, biomarkers, and genetic tests offer a broader view of the cancer’s behavior and potential risk. This combination of data can lead to a more comprehensive evaluation of the disease, aiding in the determination of whether active surveillance, immediate treatment, or a specific type of treatment is most appropriate.
Assessing Tumor Aggressiveness and Prognosis
Assessing the aggressiveness and predicting the prognosis of prostate cancer is a complex process that is crucial for guiding treatment decisions and patient management. This assessment primarily revolves around specific criteria such as the Gleason score and tumor stage, in conjunction with biopsy results.
The Gleason score remains a cornerstone in evaluating prostate cancer aggressiveness. It is determined from biopsy samples, based on the microscopic appearance of cancer cells.
“Pathologists assign a grade, ranging from 1 to 5, to the most predominant and second most predominant patterns of cells in the tissue,” says Dr. Epstein.
The sum of these grades yields the Gleason score, with higher scores indicating more aggressive cancer. This system effectively stratifies patients into risk categories, influencing treatment decisions.
Tumor stage, another vital criterion, involves determining the extent of cancer spread. Staging combines the size of the tumor (T stage), the involvement of nearby lymph nodes (N stage), and the presence of distant metastasis (M stage). Imaging tests, alongside biopsy results, contribute to accurately staging the cancer.
Biopsy results, including the Gleason score and tumor extent, are pivotal in predicting the prognosis and potential disease progression. They help in identifying patients who are suitable for active surveillance and those who require more aggressive treatment. The quality and representativeness of the biopsy are significant here, as inadequate sampling might lead to an underestimation of the tumor’s aggressiveness.
Continuous monitoring and reassessment are crucial in prostate cancer management, especially under active surveillance. Regular follow-ups involving PSA testing, repeat biopsies, and imaging are necessary to detect any changes in the tumor’s behavior. This ongoing assessment allows for timely intervention if the cancer shows signs of progression or increased aggressiveness.
Advancements in imaging, molecular biology, and genetics are poised to revolutionize how we approach this prevalent disease. As these technologies evolve, they will undoubtedly refine our ability to assess tumor aggressiveness and prognosis, leading to more effective and less invasive management strategies.