Dental claim denials are one of the biggest challenges in dental billing and revenue cycle
management. A single denied dental insurance claim can disrupt cash flow, delay
reimbursements, and create frustration for both dental practices and patients.
According to the National Association of Dental Plans, more than 70% of Americans have
dental benefits. While this increases patient access to care, it also means dental practices
must navigate complex insurance requirements. When a dental claim is denied, it impacts
revenue, administrative workload, and patient satisfaction.
This guide explains the most common reasons for dental claim denials—and how your
practice can prevent them.
Why Dental Billing Is Different From Medical Billing
Dental billing has unique coding standards, documentation requirements, and payer
guidelines. To reduce the risk of dental insurance claim denials, every claim must include
accurate and complete information, such as:
● Provider fee details
● Provider and patient demographics
● Subscriber information
● Clinical notes
● Required attachments (X-rays, periodontal charts, narratives)
● Date of initial placement (for crowns, bridges, etc.)
For official billing guidance, refer to the American Dental Association.
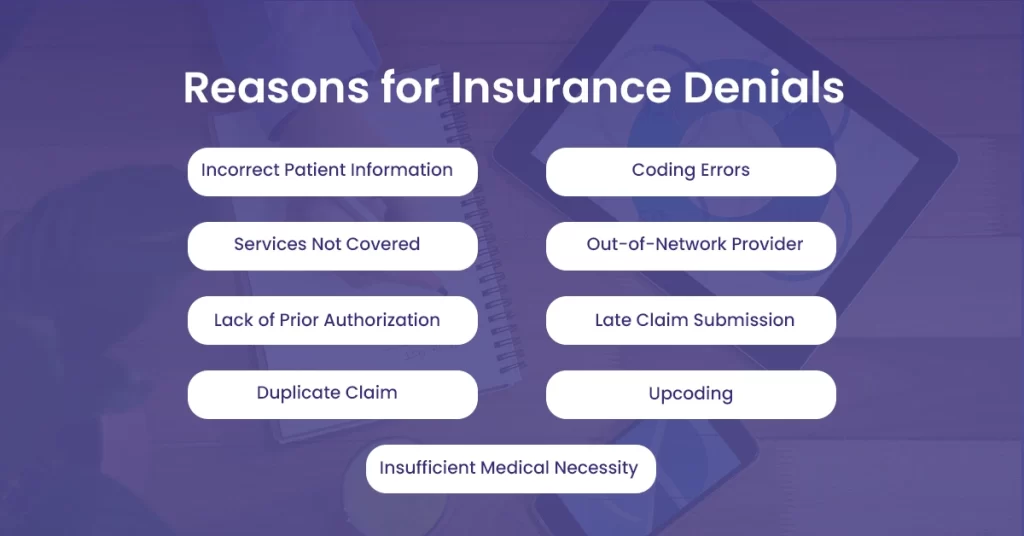
Top Reasons for Dental Claim Denial
1. Documentation Errors
One of the most common causes of dental claim denials is incorrect or incomplete
documentation. Over 50% of denied claims occur due to form errors.
Common documentation mistakes include:
● Incorrect patient information
● Missing subscriber details
● Wrong Tax Identification Number (TIN) or Employer Identification Number (EIN)
● Missing clinical notes
● Incorrect CDT codes
● Failure to attach required supporting documents
How to prevent it:
Implement a pre-submission checklist. Verify patient demographics, insurance eligibility, and
required attachments before filing.
2. Missing X-Rays or Supporting Attachments
Insurance companies often deny claims when supporting documentation is
missing—especially radiographs for procedures like crowns, root canals, and periodontal
treatment.
The California Dental Association recommends:
● Including a narrative explaining the clinical necessity
● Providing clearly labeled X-rays (patient name and date visible)
● Attaching periodontal charts when required
● Submitting printed or digital documentation in payer-approved format
If you cannot justify medical necessity, reimbursement is unlikely.
3. Use of Outdated Claim Forms
Insurance carriers frequently update their claim forms and electronic submission standards.
Submitting outdated dental claim forms can result in automatic rejection or delayed
processing.
Best practice:
Regularly verify payer requirements and ensure your practice management software is
updated to reflect current standards.
4. Late Claim Submission (Timely Filing Limits)
Most dental insurance plans have a timely filing limit, often 90 days from the date of
service. Submitting claims after the deadline typically results in denial.
However, filing deadlines vary by payer.
Prevention strategy:
● Train front desk and billing staff on payer timelines
● Submit claims daily or weekly
● Track aging reports to prevent missed deadlines
Timely filing compliance is critical to maintaining steady dental practice revenue.
5. Plan Limitations and Frequency Restrictions
Every dental insurance plan includes:
● Annual maximums
● Lifetime maximums
● Frequency limitations (e.g., two cleanings per year)
● Age restrictions
● Waiting periods
● Exclusions
Some procedures—especially major or reconstructive treatments—require pre-authorization.
Failure to verify benefits before treatment can result in denied claims.
Action step:
Always perform insurance verification prior to treatment and document benefit breakdowns
carefully.
6. Coordination of Benefits (COB) Issues
Patients with dual dental coverage often create complications during claim processing.
Coordination of Benefits errors can delay or deny payment.
Common COB mistakes include:
● Failure to submit Explanation of Benefits (EOB)
● Incorrect primary vs. secondary payer information
● Incomplete insurance data
● Submitting to the wrong carrier first
Solution:
Collect and verify both insurance policies at the initial visit. Confirm which payer is primary
and submit claims accordingly.
How to Reduce Dental Insurance Claim Denials
To improve your dental claim approval rate:
● Verify insurance eligibility before treatment
● Use correct CDT codes
● Attach required X-rays and narratives
● Monitor claim aging reports
● Stay updated on payer requirements
● Train staff regularly on dental billing best practices
A proactive billing process significantly reduces accounts receivable (AR) days and improves
cash flow.
Should You Outsource Dental Billing?
Managing dental insurance claims in-house can be time-consuming and complex. Many
practices choose to partner with a dental billing company to improve efficiency and reduce
denial rates.
A professional dental billing service can:
● Handle claim submissions
● Follow up on denied or pending claims
● Manage insurance verification
● Reduce AR days
● Improve overall revenue cycle performance
Outsourcing dental billing allows dentists and clinical teams to focus on patient care while
specialists manage reimbursements and payer communication.
Final Thoughts
Dental claim denials are preventable in most cases. By improving documentation accuracy,
verifying benefits, submitting claims on time, and ensuring proper attachments, your practice
can dramatically increase claim approval rates.
If your dental practice struggles with frequent denials, delayed reimbursements, or
administrative overload, evaluating your dental billing workflow—or partnering with
experienced dental billing professionals—may be the most strategic next step.
Reducing claim denials isn’t just about compliance; it’s about protecting your revenue and
delivering a seamless patient experience.