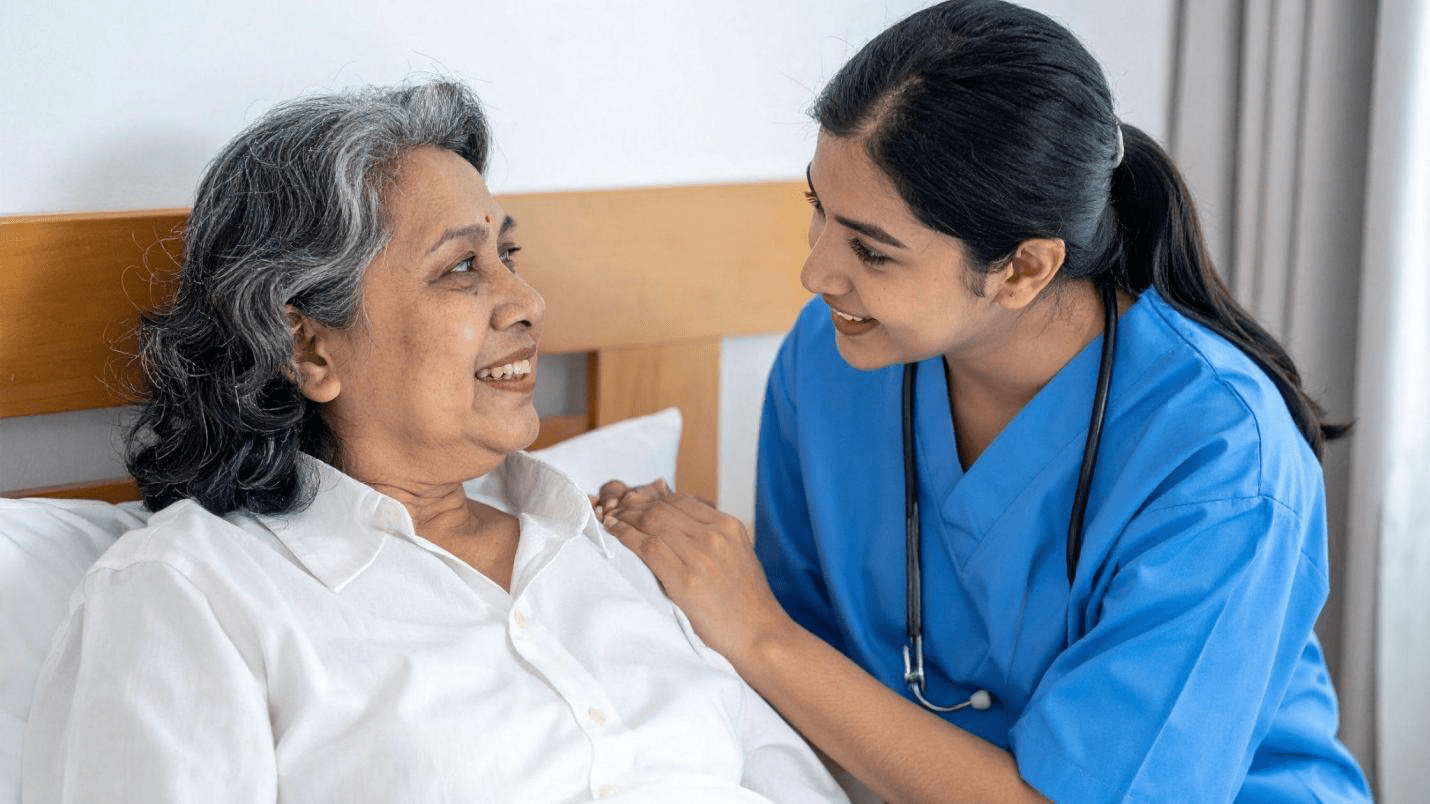
In India, many treatments now finish within a few hours, without an overnight stay. AYUSH care is also a real preference for many families. If you are comparing health insurance plans, it helps to know what is typically covered, what is restricted, and which documents help ensure smooth claims processing before you buy or renew.
In this article, you will explore what daycare and AYUSH treatments usually cover, plus the common limits and claim steps.
What Are Daycare Procedures in Health Insurance?
Here, you will explore the daycare procedures in health insurance:
Meaning in Policy Terms
A daycare procedure is completed on the same day, yet treated as hospitalisation under your policy, provided it fits the plan’s definition. Insurers look for medical necessity and a supervised clinical set-up, not the length of admission.
Why Insurers Cover Them
Because intensive procedures can still occur during a short visit, daycare coverage prevents repeated out-of-pocket expenses for treatments that no longer require an overnight stay.
What’s Typically Included under Daycare Coverage
Here are the typical daycare coverage:
Coverage Bucket
When admissible, health insurance usually pays costs that are directly linked to the daycare episode and supported by hospital records:
A Few Common Daycare Examples
Plans often cite procedures that are commonly treated as daycare, depending on your policy wording:
Common Conditions, Caps, and Grey Areas for Daycare
Daycare claims can be reduced or rejected due to common plan rules:
Daycare Claim Process: How It Usually Works
Here you will explore how it will work:
Cashless in a Network Hospital
The hospital usually sends a pre-authorisation request to the insurer or TPA with medical notes and an estimate. After approval, admissible costs are settled directly; you pay non-admissible items and deductions based on limits.
Reimbursement When Cashless Isn’t Used
If cashless is not used, you pay first and submit the claim. The insurer reimburses the admissible portion in accordance with the policy terms.
Documents Typically Required for Daycare Claims
Most insurers ask for:
AYUSH Coverage in India: What It Usually Means
AYUSH covers Ayurveda, Yoga, Naturopathy, Unani, Siddha, and Homoeopathy. In many policies, AYUSH cover is primarily for inpatient treatment at recognised AYUSH hospitals or centres, not for routine wellness or casual OPD expenses.
What’s Typically Included under AYUSH Hospitalisation
When an AYUSH admission is admissible, plans commonly cover:
Key Conditions and Common Exclusions for AYUSH
AYUSH benefits typically come with these checks:
How Daycare and AYUSH Benefits Interact with Your Sum Insured
In many health insurance plans for families, daycare and AYUSH claims reduce the base sum insured, which can affect the coverage available later. Waiting periods and pre-existing condition rules may apply, and exclusions or caps can change the final settlement.
Closing Note
Daycare and AYUSH coverage can make health insurance for family decisions more meaningful, but only when the hospital, treatment type, and policy limits align. Read the wording, confirm eligibility in advance, and keep records organised. Also, ask the hospital for a clear estimate and pre-authorisation support to avoid surprises at discharge.