Most people have experienced an ocular migraine’s unsettling visual disturbances that appear unexpectedly. These frightening episodes can fill your vision with zigzag lines, blind spots, and flashing lights. Many people mix up ocular migraines with vestibular migraines, though each affects our bodies differently.
The visual migraine symptoms cause temporary changes in vision, and ocular migraine aura effects vary considerably. Vestibular migraine symptoms typically manifest as vertigo, balance problems, and spatial disorientation rather than visual disturbances. The ability to distinguish between vestibular and ocular migraine symptoms is significant for effective treatment and management. If you’re experiencing recurring episodes, consulting a specialist at a migraine clinic Brisbane can help determine which type you’re dealing with. In this piece, we’ll examine these two types of migraines’ key differences, their distinct symptoms, and the medical professionals’ approach to diagnosis and treatment.
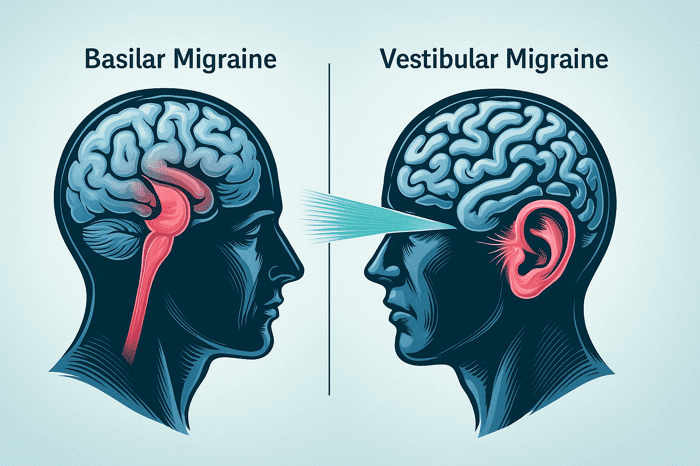
What is the difference between vestibular and ocular migraines?
Ocular and vestibular migraines show clear differences in how they affect the body and what symptoms they create.
Ocular migraines target the visual system and cause temporary sight problems in one eye. These visual symptoms range from blind spots to flashing lights or scotomas. The visual changes from ocular migraines usually lead to headaches within an hour. On top of that, these sight issues don’t last long and might show up with or without the typical migraine headache.
The balance system takes the hit with vestibular migraines that bring on dizziness, vertigo, and problems with balance. Vestibular migraines stand out as the main neurological reason behind occasional vertigo. Research shows women face this condition 1.5 to 5 times more often than men.
A vital difference shows that vestibular migraines don’t always come with headaches. These symptoms can stick around much longer, anywhere from minutes to days. Doctors look for at least five episodes with balance-related symptoms that are moderate to severe and last between 5 minutes and 72 hours to make a diagnosis.
Both types of migraines can substantially affect daily life. Moderate vestibular symptoms make daily tasks harder but still possible, while severe symptoms stop activities completely. Though both fall under the migraine umbrella, knowing their unique features helps ensure the right diagnosis and treatment plan.
Symptoms: How do they show up differently?
Understanding symptom patterns helps identify which type of migraine you experience.
Ocular migraines cause visual disturbances that affect one eye and last 10 to 20 minutes. Patients see temporary blind spots, zigzagging patterns, shimmering lights, and floating lines. Half of all patients lose vision completely in one eye, while 20% notice blurring, and 13% develop scotomas. The headache usually strikes behind the affected eye and makes patients sensitive to light, noise, and odours.
Vestibular migraines demonstrate different characteristics and affect balance instead of vision. Vertigo becomes the main symptom, which patients describe as a “to-and-fro” sensation. People who suffer from these migraines experience sudden episodes of dizziness, imbalance, and spatial disorientation. Research shows 30% of people with vestibular migraines might never have experienced headaches.
Each type follows distinct timing patterns. Visual issues from ocular migraines last 5-60 minutes, but the headache can continue 4-72 hours without treatment. Vestibular migraine attacks range from minutes to days. Patients who experience attacks between midnight and noon often report more severe symptoms.
Vestibular migraines can also trigger cochlear symptoms like aural fullness, tinnitus, and hearing fluctuations. These symptoms never appear in ocular variants.
Diagnosis and treatment options
Doctors need an accurate diagnosis to start effective treatment for ocular and vestibular migraines.
Healthcare providers diagnose vestibular migraines through neurological examinations, videonstagmography or electronystagmography, and imaging tests like CT scans. Diagnosis becomes especially challenging when vestibular migraine symptoms don’t align with headaches.
Doctors can confirm ocular migraines by observing reduced blood flow to the patient’s eye during an episode.
Both conditions share several treatment options. Patients can take these medications for acute attacks:
- Paracetamol, NSAIDs (ibuprofen, diclofenac), and triptans (sumatriptan)
- Antiemetics to relieve nausea
Doctors usually prescribe these preventive medications:
- Beta-blockers (propranolol, metoprolol)
- Calcium channel blockers (verapamil)
- Antiepileptics (topiramate, valproate)
- Antidepressants (amitriptyline, venlafaxine)
An all-encompassing approach works best alongside medication. Studies show that patients experience fewer symptoms when they make lifestyle changes. These changes include:
- Regular sleep patterns
- Daily exercise
- Avoiding trigger foods (alcohol, caffeine, MSG, chocolate)
- Fixed meal times
Vestibular physiotherapy helps patients with vestibular migraines significantly. The most effective strategy combines preventive medication, lifestyle changes, and acute treatment options.
Conclusion
The way vestibular and ocular migraines affect people is different, and this makes a big difference in how we manage these conditions. Both are types of migraines, but they demonstrate distinct symptoms that affect different body systems.
Ocular migraines affect vision with temporary issues like zigzag patterns and blind spots that usually last less than an hour. But vestibular migraines target the balance system and cause vertigo and spatial disorientation that can last for days. On top of that, it’s common to feel headaches behind the eye during ocular migraines, while vestibular migraines might not cause any head pain at all.
The way doctors diagnose these conditions varies too. They check for reduced blood flow to the eye during ocular episodes. A vestibular migraine diagnosis needs a complete neurological exam with specialised tests. Notwithstanding that, both conditions respond to similar treatments that combine acute medications like triptans with preventative drugs such as beta-blockers.
Lifestyle changes are a vital part of managing these conditions. A good sleep schedule, regular meals, and knowing your triggers can reduce how often and severe these episodes become. People with balance-related symptoms can benefit from vestibular physiotherapy.
Getting the right diagnosis is the foundation to find effective treatment. Many people don’t get the help they need because of wrong diagnosis or mix-ups between these conditions. If you keep having visual problems or unexplained vertigo episodes, you should ask a healthcare professional to identify and manage your specific migraine type. The right diagnosis guides you to the right treatment and ended up giving you a better quality of life.