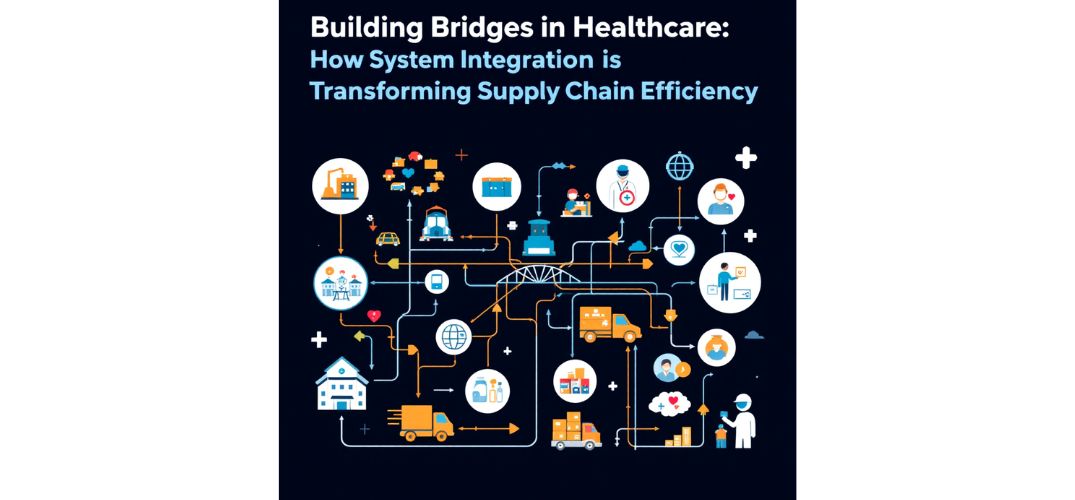
In this modern era, enterprise integration is revolutionizing medical supply networks, reshaping healthcare delivery with precision and innovation. Ajay Mutukula, a recognized voice in healthcare systems research, explores the transformative power of enterprise integration in medical supply networks. With technical precision and insight, he outlines how innovation is reshaping healthcare delivery at its operational core.
A Network of Necessity
Modern healthcare operates in a high-stakes environment where precision, safety, and speed are non-negotiable. At the heart of this complexity lies the supply chain—a web managing everything from surgical masks to specialized biologics. Yet, this has long been fragmented. Integration is no longer optional; it’s the engine driving reliable care and resilience. By linking clinical workflows to backend operations, system integration bridges gaps that historically led to inefficiencies, data silos, and delayed treatments.
The Symphony of Systems
Enterprise Resource Planning (ERP), Warehouse Management Systems (WMS), Electronic Health Records (EHR), and Transportation Management Systems (TMS) form the backbone of healthcare logistics. When functioning in isolation, the result is duplicated data, manual errors, and delays. But when orchestrated through seamless integration, they enable predictive restocking, tracking precision, and real-time visibility. Integrating EHRs with supply platforms ensures that inventory aligns with care schedules, reducing emergency restocking and improving forecasts.
API-First: The Language of Modern Integration
RESTful and FHIR-based APIs are now the preferred architecture for integration. These APIs, built for scalability and speed, allow organizations to deploy solutions quickly and adapt as needs evolve. Their lightweight, JSON-based structures reduce bandwidth and increase efficiency. Security features like OAuth 2.0 and near real-time data exchange make APIs indispensable in dynamic healthcare settings.
EDI and Events: Time-Tested Tools Meet Modern Demands
Despite API advancements, Electronic Data Interchange (EDI) still processes most healthcare transactions. Secure protocols like AS2 and strong validation frameworks ensure data reliability. Event-driven architectures, meanwhile, elevate responsiveness. Systems that react to stock-out alerts or temperature anomalies can prevent costly disruptions and improve outcomes, shifting operations from periodic to proactive.
Standardizing for Safety
Adoption of GS1 standards—Global Trade Item Numbers (GTIN), Global Location Numbers (GLN), and Serial Shipping Container Codes (SSCC)—has revolutionized traceability and compliance. These identifiers create a shared language across manufacturers, distributors, and providers. With GS1, the risks of mislabeling, delivery errors, and regulatory issues decline. EPCIS frameworks support event-based product tracking, amplifying lifecycle traceability.
Clinical and Supply Chain Convergence
Integrating HL7 and FHIR standards into the supply chain marks a critical evolution. These standards connect clinical events to supply consumption, enabling accurate cost capture and optimization. Automated charge capture based on procedure data minimizes manual entry, enhancing both financial accuracy and efficiency. Standardized location hierarchies bridge physical spaces with digital systems, ensuring timely product delivery.
Foundations of Reliability: Master Data and Security
Effective integration starts with trustworthy data. Master data management ensures consistency across platforms—from product attributes to supplier info. Without this, even advanced integrations falter. On the security front, layered defenses—end-to-end encryption, role-based access, audit logging—safeguard sensitive data. As cyber threats grow, these frameworks prevent breaches that could disrupt healthcare systems.
Testing for Resilience
Integration is not just about connection it’s about reliability under stress. Testing must simulate real-world pressures, including transaction peaks and system failures. Fault-injection testing, volume testing, and comprehensive validation protocols reduce post-launch issues and ensure continuity. In healthcare, where downtime can compromise care, these safeguards are essential.
Emerging Frontiers: Blockchain and AI
Blockchain brings new levels of trust and verification to healthcare supply chains. From immutable custody records to compliance via smart contracts, blockchain reduces fraud and eases audits. Meanwhile, AI transforms the supply chain with advanced analytics, predictive maintenance, and intelligent forecasting. Machine learning models enhance decisions by predicting demand and spotting anomalies in temperature-controlled logistics.
In conclusion, as demands on healthcare systems grow, integration stands as a defining capability for operational excellence. The fusion of clinical and supply data enables not just smoother operations, but smarter, safer care. Ajay Mutukula’s exploration shows that integration is more than an IT upgrade; it is a strategic transformation. For organizations striving to lead in care and efficiency, the path lies in mastering seamless, secure, intelligent system integration.