When considering dental fillings—composite, amalgam, gold, or ceramic—their immediate benefits often take center stage. However, the long-term effects of these materials on systemic health deserve more attention. Dental materials interact with biological tissues over extended periods, and understanding their potential impact is crucial for ensuring patient safety and well-being.
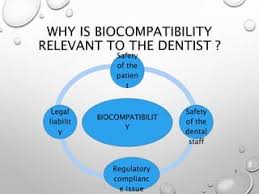
What Is Biocompatibility?
Biocompatibility refers to a material’s ability to function in the body without causing harm. Dental materials undergo rigorous testing before approval, but their long-term systemic effects remain an area of ongoing research. While acute reactions such as localized irritation or allergic responses are relatively well-documented, subtle chronic effects, including potential links to autoimmune diseases or endocrine disruptions, require further investigation.
Common Filling Materials and Their Long-Term Effects
1. Amalgam
Amalgam fillings, a mixture of mercury, silver, tin, and copper, are widely used due to their durability and cost-effectiveness. However, the presence of mercury has sparked concerns about neurotoxicity and systemic health effects. The American Dental Association and the FDA assert that the mercury exposure from amalgam fillings is within safe limits. Yet, some studies suggest that cumulative exposure over decades could contribute to subtle neurological or immune system disturbances in susceptible individuals. Mercury hypersensitivity, though rare, can lead to symptoms like skin rashes, fatigue, and cognitive difficulties.
2. Composite Resins
Composite resins, favored for their aesthetic appeal and versatility, are made of a blend of plastic and glass particles. While they provide a natural look and strong adhesion, concerns have been raised regarding the potential release of bisphenol A (BPA) and other endocrine-disrupting chemicals. BPA exposure, even in trace amounts, has been linked to hormonal imbalances, metabolic disorders, and reproductive health concerns. Although modern composite formulations have minimized BPA content, long-term exposure to these materials requires further research to determine any cumulative systemic effects.
Must Read: https://tododisca.com/
3. Ceramic Fillings
Ceramic fillings, including porcelain and zirconia, are known for their biocompatibility and resistance to wear. They do not contain metals or BPA, making them a preferred choice for patients with sensitivities. However, rare cases of allergic reactions to trace elements, such as aluminum oxide or other ceramic stabilizers, have been reported. Additionally, the long-term mechanical properties of ceramics in high-stress areas of the mouth need ongoing evaluation to ensure they maintain their integrity over time.
4. Gold Alloys
Gold alloy fillings are highly durable and exhibit excellent biocompatibility. They do not corrode and rarely cause adverse reactions. However, certain gold alloys contain trace amounts of nickel, palladium, or other metals that may trigger allergic reactions in sensitive individuals. While these cases are uncommon, they underscore the importance of personalized material selection for dental restorations.
Areas for Further Research
1. Rare Allergies
While most dental materials are considered safe, individual hypersensitivities can lead to adverse reactions. Nickel sensitivity, for example, is a well-documented condition that can result in dermatitis or systemic inflammatory responses. Research into genetic predispositions to material allergies could help identify at-risk patients before placing specific restorations.
2. Systemic Conditions
The relationship between dental materials and chronic illnesses, including autoimmune diseases, remains an area of uncertainty. Some anecdotal reports suggest that metal-based fillings may contribute to immune system dysregulation in susceptible individuals, but conclusive evidence is lacking. Ongoing epidemiological studies are needed to clarify these potential links.
3. Cumulative Exposure
Repeated low-level exposure to substances like mercury (from amalgam) and BPA (from composite resins) over decades is another concern. While short-term studies indicate safety, the effects of prolonged exposure across a lifespan have not been fully explored. Research into cumulative toxicology and bioaccumulation will provide a clearer understanding of whether these materials pose long-term health risks.
Looking Ahead: The Role of Personalized Dentistry
Dr. Sehat, who leads Dentology Dentistry of Irving, TX, emphasizes that patients should actively discuss their material options with their dentist, particularly if they have known allergies, systemic conditions, or concerns about biocompatibility. Advances in dental biomaterials are leading to the development of safer, more inert options that minimize systemic risks.
Personalized dentistry, which considers a patient’s unique biological makeup, could play a key role in optimizing treatment choices. In the future, genetic testing and biocompatibility assessments may become standard practice, ensuring that each patient receives the most suitable and health-conscious dental restorations.
Conclusion
While current dental materials are generally regarded as safe, knowledge gaps remain regarding their long-term effects on systemic health. As scientific understanding evolves, continuous research and technological advancements will be crucial in addressing these concerns. Patients are encouraged to stay informed, ask questions, and work collaboratively with their dental professionals to make educated decisions about their oral and overall health.